The American Urological Association (AUA) 2013 national meeting remains in full swing in beautiful San Diego. Not sure what is going on with the weather (two days in a row of rain?), but plenty of great things going on inside the convention center.
The American Urological Association (AUA) 2013 national meeting remains in full swing in beautiful San Diego. Not sure what is going on with the weather (two days in a row of rain?), but plenty of great things going on inside the convention center.
The “main event” on Monday was Dr. Ballentine Carter’s presentation of the AUA’s new Guidelines on the Early Detection of Prostate Cancer . Dr. Carter spoke to a packed house (the Fire Marshall was turning people away!).
For those who missed the talk, the AUA added a second session on Tuesday. Further comments from the AUA can be found here. Whatever your opinion regarding the new guidelines, and there were many prominent urologists who voiced their concerns about the guidelines, urologists will need to be able to speak intelligently to patients and primary care physicians. In the same session, Dr. Michael Cookson gave the AUA Guideline presentation on castration resistant prostate cancer which seemed better received than the PSA Guidance which certainly got many urologists hot and bothered.
On Monday, the Young Urologists Forum focused on the business aspect of urology (something I heard very little about in training), with informative talks by Dr. Raju Thomas, Dr. Koushik Shaw and Dr. Neil Baum. Thanks to Dr. Mike Ost and the YU Committee for putting together a great program.
Speaking of young urologists, the Southeastern section took home first prize in the Second Annual Residents Bowl, besting the Western section in the finals on Monday.
 Southeastern Section of AUA claim the honours in the Annual Residents Bowl
Southeastern Section of AUA claim the honours in the Annual Residents Bowl
The Monday plenary session included discussions on the contemporary uses of neuromodulation and the management of iatrogenic ureteral injury. BJUI Editor-in-Chief Dr. Prokar Dasgupta, gave an informative lecture on the current applications of botulinum toxin in the lower urinary tract. Prostate cancer made it into the Endocrine Forum on Monday, with Dr. Scardino and Dr. Klotz debating the treatment of men with low risk prostate cancer. Jumping ahead, a similar debate was held during the Tuesday plenary between Dr. Carroll and Dr. Tewari with roles reversing somewhat as Dr Tewari argued the case for surveillance while Dr Carroll took us through some of the pitfalls.
Also on Monday, Dr. Vincent Laudone gave late-breaking news regarding the randomized trial between open and robotic radical cystectomy at MSKCC. Bottom line – no difference was found regarding oncologic or perioperative outcomes. In particular, the robotic approach did not reduce the complication rate which remained at about 60% in both arms. Cost difference, which seems to be on everyone’s mind, was not addressed. Other trials between open and robotic cystectomy remain ongoing and the jury appears out here.
Dr. Christopher Kane moderated a session debating the use of simulation in robotic surgery between Drs. Sundaram (pro) and Nadler (con). Dr. Kane concluded the debate by stating that basic robotic training is important but limited by cost and duty hour restrictions. In addition, further studies are needed to determine if virtual robotic training actually helps performance.
One of the more contentious areas of prostate cancer, HIFU and focal therapy, received much attention during various poster sessions this year. Abstract #553 reported five-year oncological outcomes following HIFU in the UK in over 500 patients. Disappointingly, 38% of men who had a biopsy had residual cancer. About one third of patients had androgen deprivation therapy upfront with a further 30% requiring salvage treatment. The authors described the disease-free outcomes as “reasonable”. Abstract #1356 from the same authors reported outcomes in 110 patients undergoing focal therapy using the same HIFU technology. Again, 38% of patients had a positive biopsy. Both of these papers provoked much reaction from the floor and across social media. These are experimental interventions which should only be undertaken in appropriate trials.
The aging US population (10,000 people turn 65 every day and will for the next 15 years) coupled with the average age of urologists (mid-50’s!) will create a serious manpower shortage over the next several years. As an illustration, abstract #153 reported that 14 counties in Oregon have zero urologists and men in those counties are more likely to get bladder cancer.
From Monday, abstract #1041 (awarded best poster for MP40), confirmed what habitual coffee drinkers already know – that high dosage coffee increases LUTS and urine volume compared to decaffeinated coffee or water. Dr. Tom Walsh and colleagues were awarded best poster (abstract #1241) for MP46 for evaluating a smartphone application to assess the penile deformity in men with Peyronie’s disease. Another best of session – Dr. Penson (@urogeek) and colleagues reported that men with prostate cancer today (CAESER) have more baseline dysfunction that men 20 years ago (PCOS) – abstract #449. There were many more great abstracts out there…too many to list in this blog.
The Urological Society of Australia and New Zealand hosted a great reception on Monday night. Several prominent uro-twitterati (including yours truly) and other urologic “heavy hitters” were in attendance.
 Thanks to the Aussies and Kiwis for a wonderful event. Strangely, they were not serving Foster’s at the event.
Thanks to the Aussies and Kiwis for a wonderful event. Strangely, they were not serving Foster’s at the event.
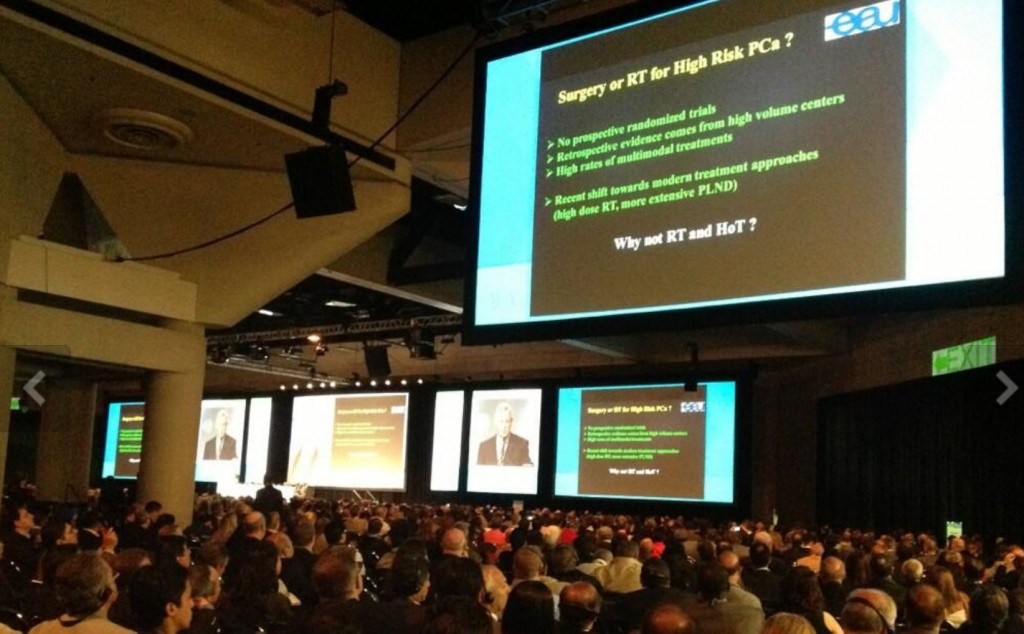
Tuesday’s plenary included several sessions on the management of both low and high-risk prostate cancer. The main auditorium was absolutely packed for what was one of the best sessions of the week.
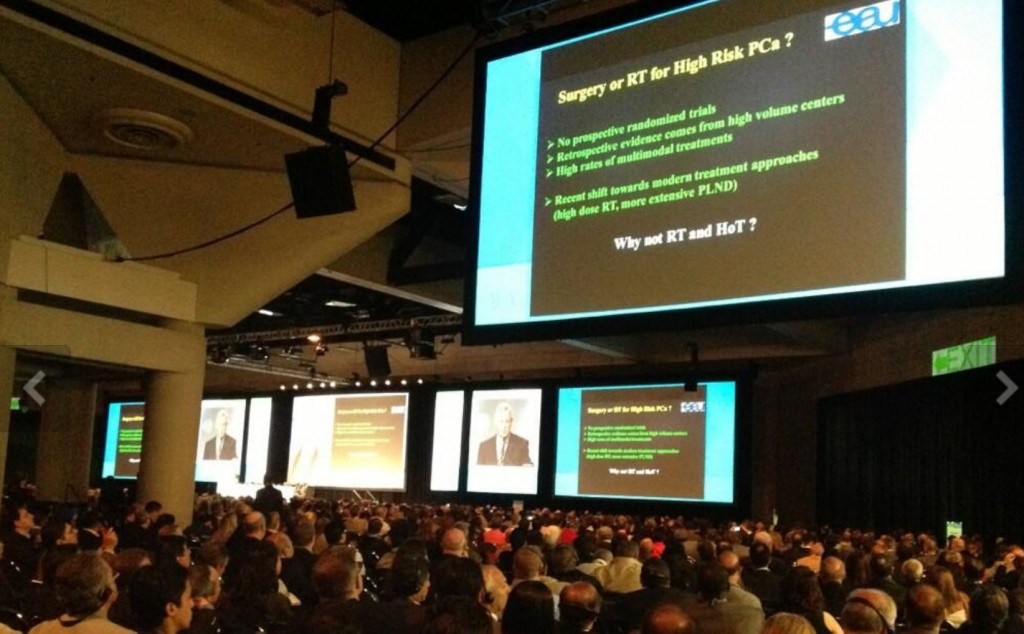
Dr Hein Van Poppel, Secretary-General Adjunct of the European Association of Urology (EAU), delivered an outstanding plenary on the management of high-risk localised prostate cancer. His clear message – surgery should always be considered first with radiotherapy and androgen deprivation therapy later if required – was very well received. Dr Ed Messing introduced a fantastic session on molecular markers in prostate cancer led by Dr’s Alan Partin, Dan Lin and Theo Van der Kwast. Key messages here were that the Phi test already has a role in clinical practice; PCA3/TEMPRSS2ERG fusion is emerging; and for sure, we will see genetic markers in clinical practice very soon. In fact the UCSF group generated a lot of media headlines on Tuesday evening when the commercialization of their genetic test was announced ahead of its presentation by Dr Cooperberg on Wednesday am.
So many other sessions it’s hard to know what to choose from. A mention of Dr Joel Nelson’s Critical Discussion session where he led Dr Reiter and Dr Brooks through the options for patients with progressive prostate cancer. This was a good way to present the key data in an engaging manner.
The AUA Guideline presentations on follow-up care for renal cancer and radiation after prostatectomy were given by Dr. Sherri Donat and Dr. Richard Valicenti, respectively. In addition, Drs. McVary and Kaplan debated the use of alpha blockers versus PDE5 inhibitors for BPH/LUTS.
Other highlights from Tuesday from the land of stones included abstract #1816 – people are 67% less likely to file short-term disability when treated with medical expulsive therapy versus ureteroscopy. A higher physical activity level improves the results of lithotripsy (#1824). In an earlier abstract (#67), physical activity was protected against stones in women. SO…get moving people! Lastly, 2 groups developed nomograms to predict stone-free rates after PCNL (abstracts #1526 and 1532). Thanks to Peter Steinberg and Michelle Semins (my stone peeps) for vetting abstracts.
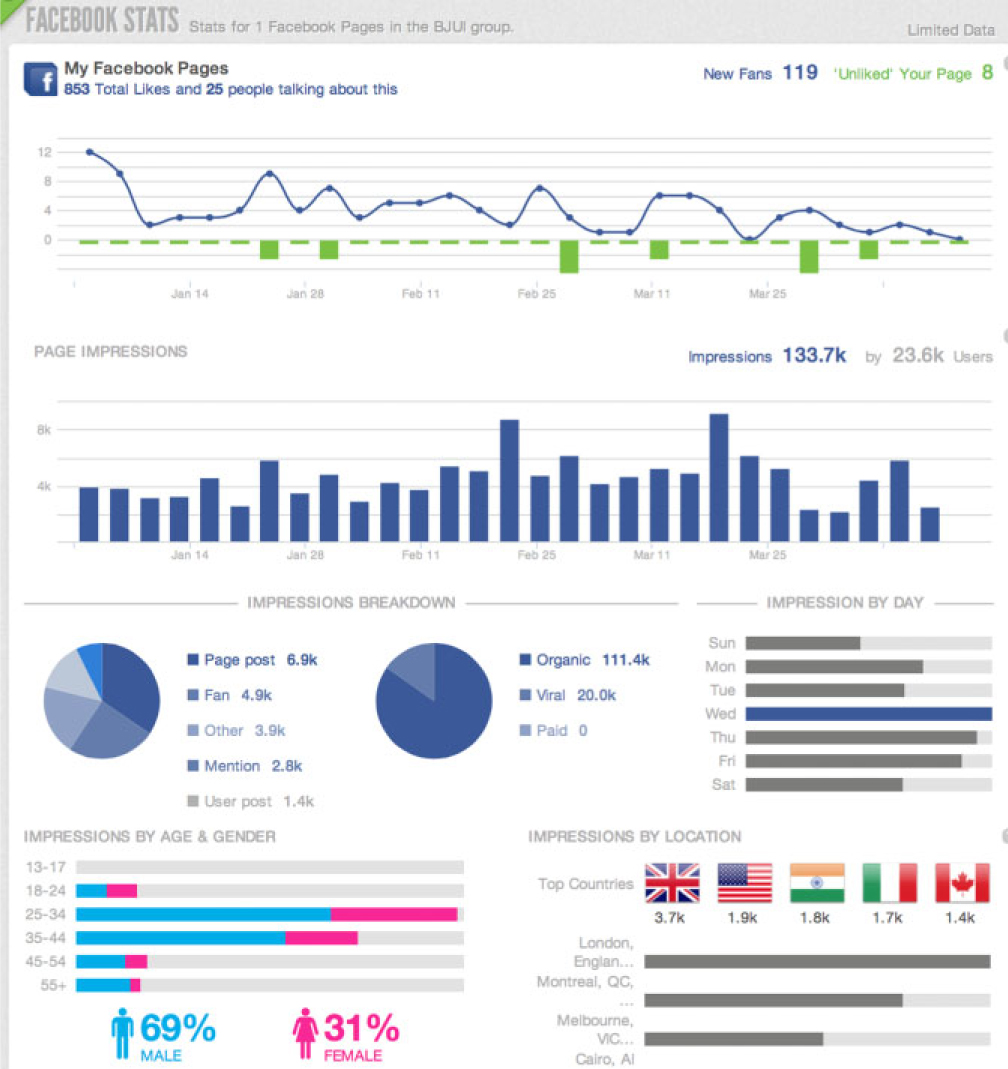
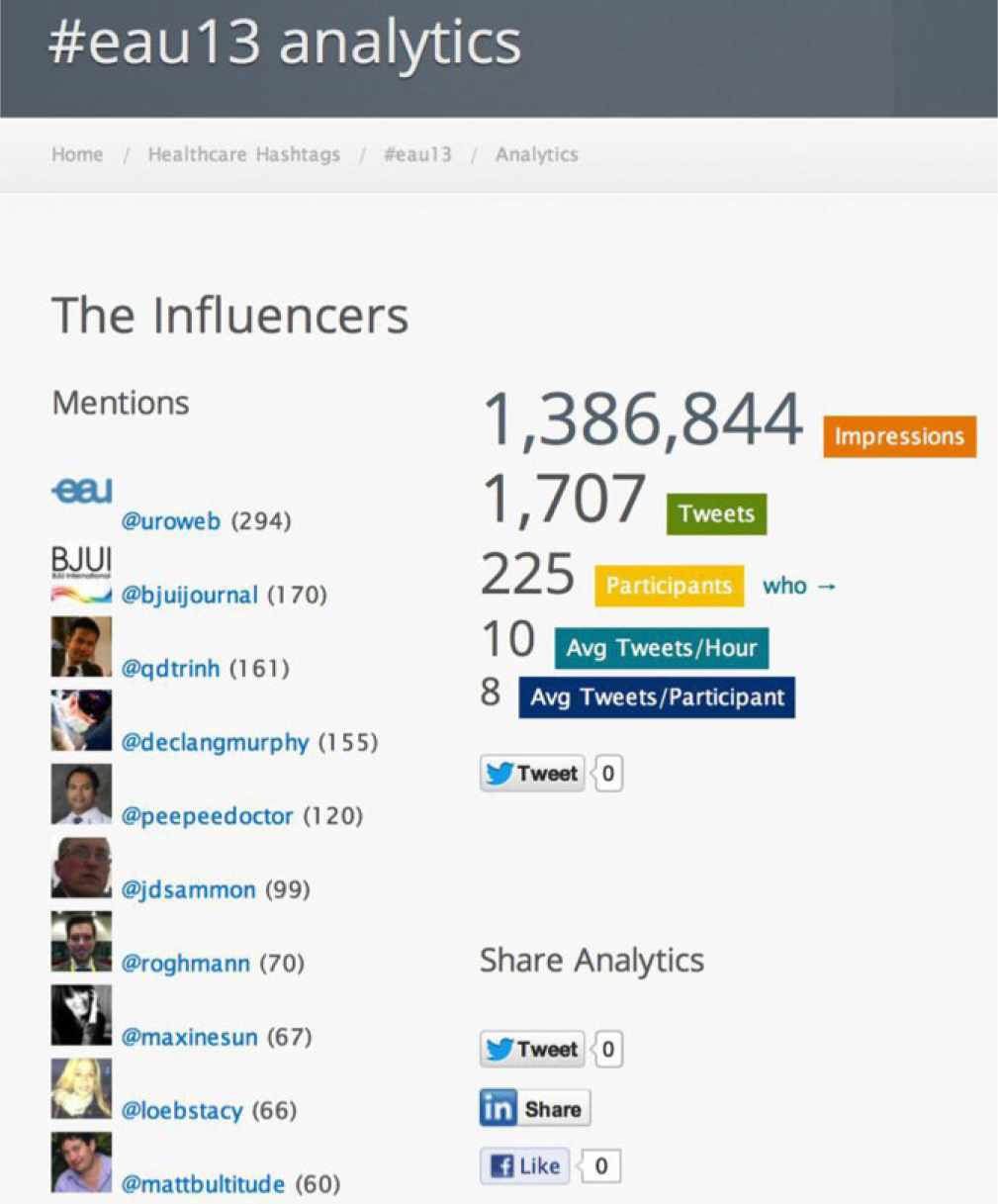
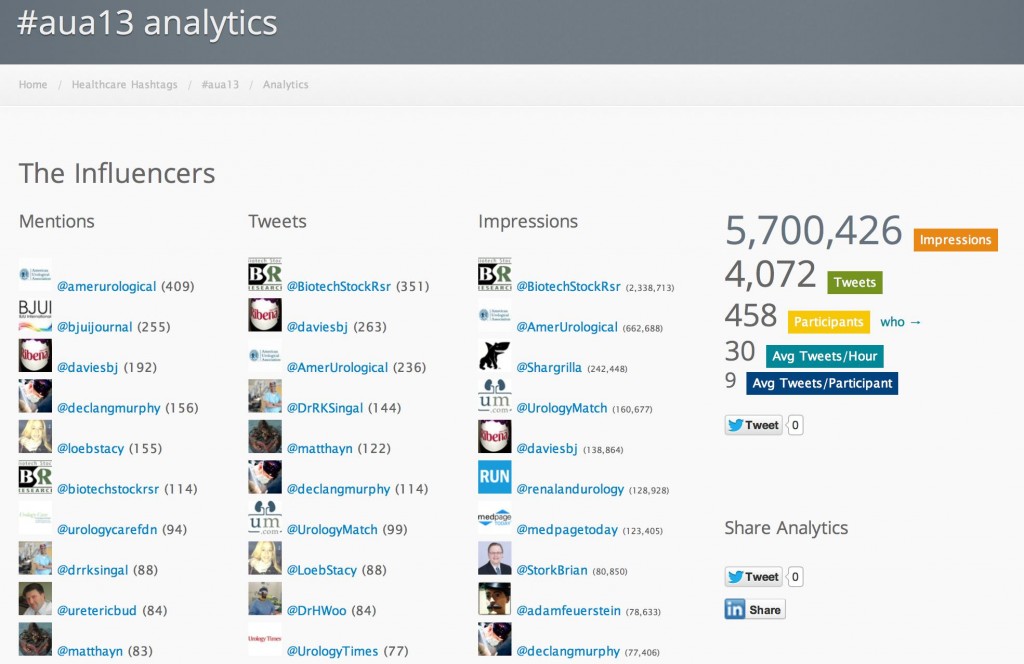
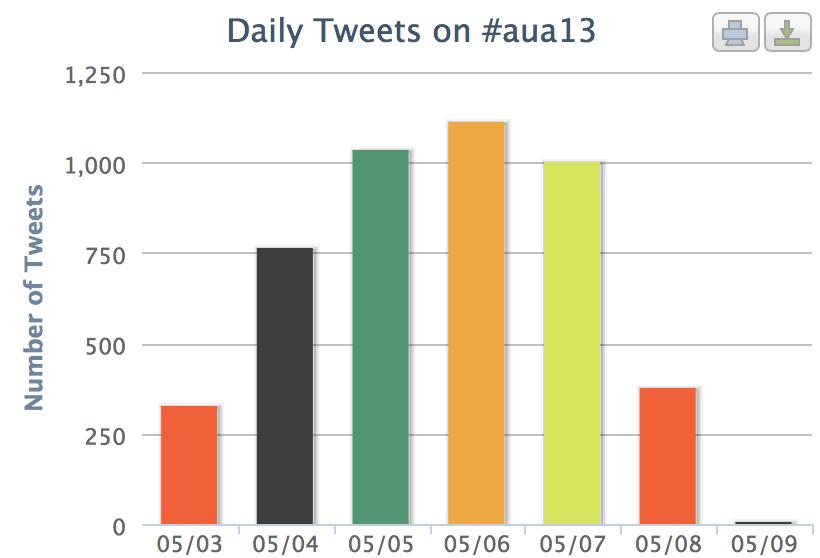
Social media and twitter continued to have a significant impact at the meeting, with an increasing number of tweets every day. With so much going on at the AUA (seemingly at the same time), twitter provides an easy way for urologists to digitally multitask and get more out of the conference. Check out the metrics via Symplur.com which show huge social media activity (5.7m digital impressions) and also shows the BJUI and its team/contributors are among the top influencers once again.
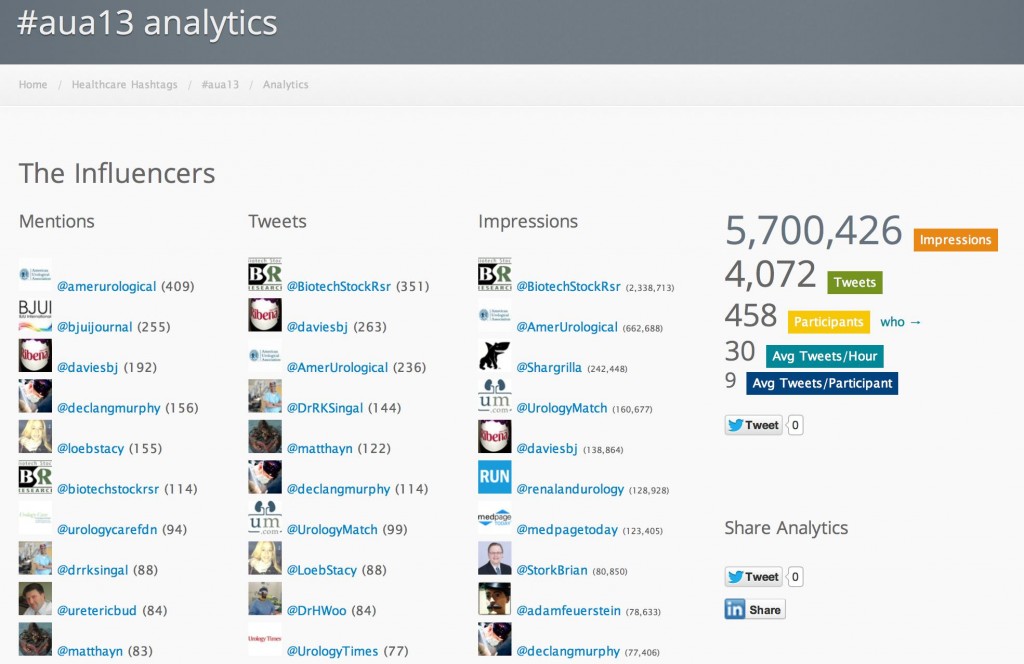
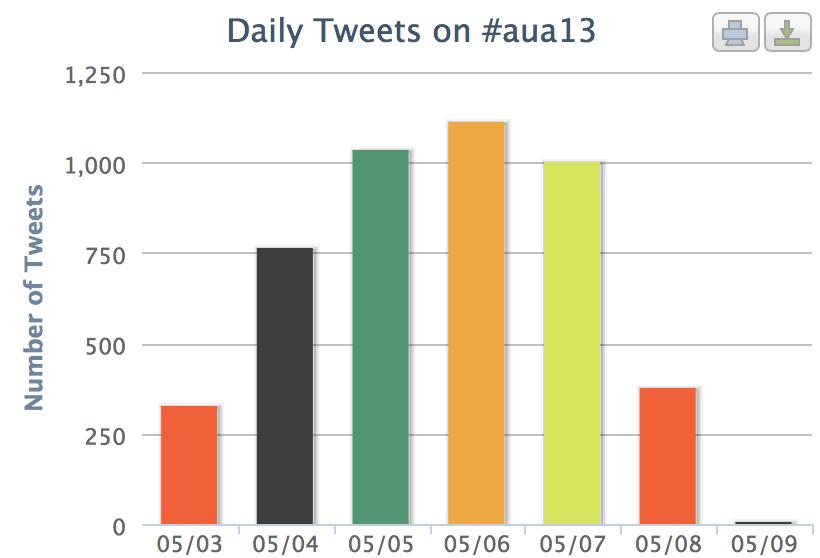
#aua13 was the #1 trending conference over the past few days! The use of social media will only expand over the coming years, and urologists need to stay “ahead of the curve”. Perhaps the @Americanurol will offer a Plenary session on Social Media next year? I can honestly say that I got more out of the meeting this year, largely thanks to the use of twitter.
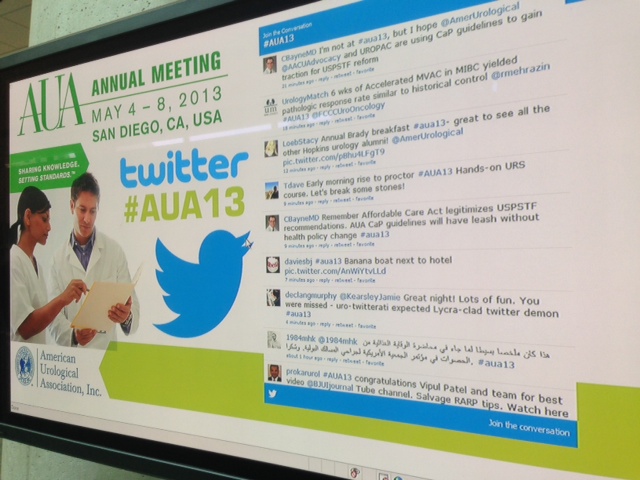
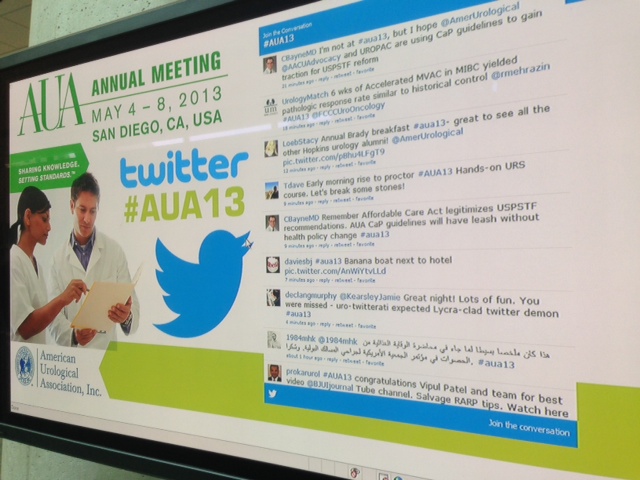 The AUA responded to a social media campaign and installed twitter-boards around the convention centre. Great to see the AUA engaging so well in social media.
The AUA responded to a social media campaign and installed twitter-boards around the convention centre. Great to see the AUA engaging so well in social media.
Thanks to the AUA and San Diego for a great meeting! Looking forward to seeing everyone next year in Orlando. Until then, I encourage everyone to participate in the International Journal club on twitter (@iurojc) and to bring a friend!
Dr. Matthew Hayn
Follow Matt on Twitter @matthayn
Comments on this blog are now closed.
 Wikipedia defines social media as a means of interactions among people in which they create, share, and exchange information and ideas in virtual communities and networks.
Wikipedia defines social media as a means of interactions among people in which they create, share, and exchange information and ideas in virtual communities and networks.