EAU Annual Meeting 2013 – Final thoughts
The BJUI team was most impressed with this year’s EAU Annual Congress which has just concluded in Milan. The scientific content was excellent – topical plenary sessions from key opinion leaders; lively poster sessions; superb video sessions and very high-quality courses run by the European School of Urology. The EAU are to be congratulated on consistently raising the bar with the quality of this meeting which is reflected in the huge delegate numbers again this year.
The last two days had a number of highlights, some of which we summarise here:
- The Plenary on lower urinary tract symptoms – management of side-effects included a wide variety of presentations including an specific talks on new potential drug treatments which certainly wouldn’t be considered main-stream at the moment. It will be interesting to monitor how trials with beta-3 agonists, botulinum toxin and PDE5 inhibitors go over the next few years for this potentially huge market. Professor Marberger finished the session discussing if TURP remains the gold standard for BPO. The answer may be that it is not, although it remains the ‘reference’ to which all other treatments must match. It is interesting to see how delegates reacted to this on Twitter such as Dr GomezSancha who tweeted to his 251 followers:
We are not sure if all would agree but we do enjoy seeing the debate bouncing around the Twittersphere!
- Prevention of infections – chaired by T.E. Bjerklund Johansen, this plenary updated us on resistance to antibiotics which is increasingly a problem and has led the lay press to describe this as an Apocalypse and more recently as big a risk as terrorism. Dr Kahlmeter then discusses the implications for urology in this video interview with the EAU. This is a highly topical area and we are pleased to see key urology meetings showing leadership here to address these broad concerns.
- Urological Surgery in Renal Transplant Patients – this session was very emlightening for urologists who work alongside bust renal transplantation services. The transplant population have many challenging urological issues and Dr Jon Olsburgh from Guy’s & St Thomas’ in London provided an excellent overview of some of these. He outlined very nice strategies for stones in patients who have received an allograft and also for those considering kidney donation. A summary can be found in the EUT Newsletter from Day 3.
- There were many poster sessions throughout each day – too many to be honest for us to keep track of. Fear not though – keep an eye on the BJUI blogs for the Best of the Best Posters coming soon. We would also direct you to Twitter where you will find some excellent commentary from the many active Tweeters who attended various poster sessions. Just search under the #eau13 hashtag. Watch out in particular for tweets from the Montreal/Detroit group who presented much work and were particularly active on Twitter (@qdtrinh, @peepeedoctor, @jdsammon, @maxinesun and others).
- Souvenir Session and EAU Guidelines on Live Surgery: The last day featured an excellent souvenir session which overviewed some of the key messages for the meeting. European Urology Editor-in-Chief Elect , Jim Catto, reviewed Urothelial cancers and observed that PET scanning has most value for evaluating distant disease rather than pelvic lymphadenopathy when compared to CT scanning. The management of small renal masses, a dominant topic this year, also . The highly-anticipated EAU Guidelines on Live Surgery were presented very nicely by Section Chairman Keith Parsons and were very well received. There are sometimes competing goals here and these guidelines will ensure that the best interests of patients are maintained while maximising the educational value of these very popular sessions.
- Breaking News: this final session had a number of headlines, one of which was data from Peter Wiklund’s group in Sweden which suggested that long-term cancer outcomes for localised prostate cancer patients are better for those who underwent surgery rather than radiotherapy. Also data from Bertrand Tombal showing a greater than 50% reduction in cardiovascular morbidity for patients on the GnRH antagonist degarelix when compared with those on GnRH analogues. Further detail of this are awaited.
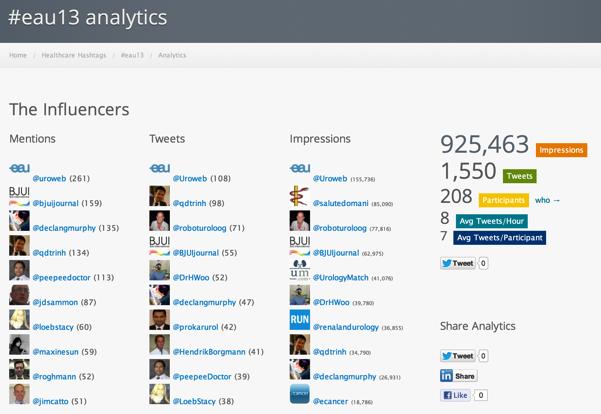
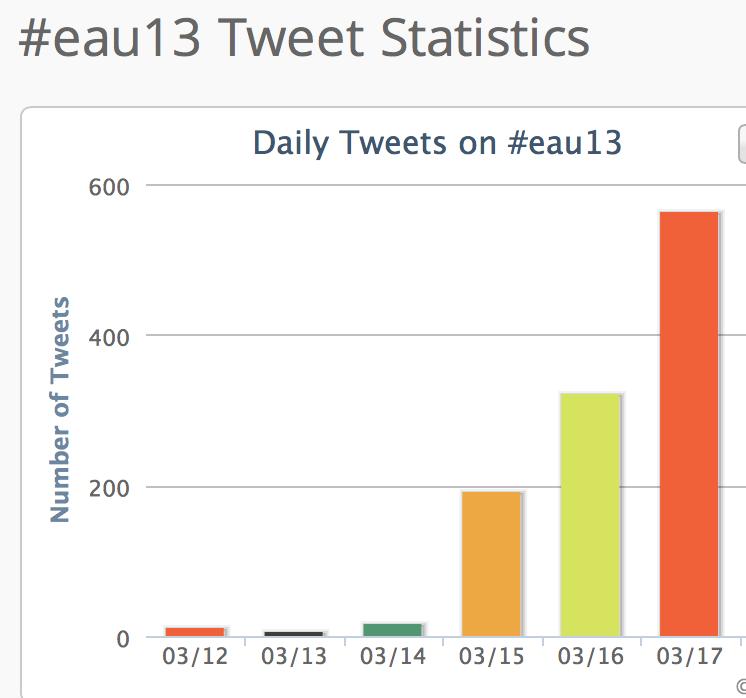
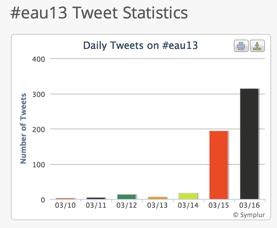
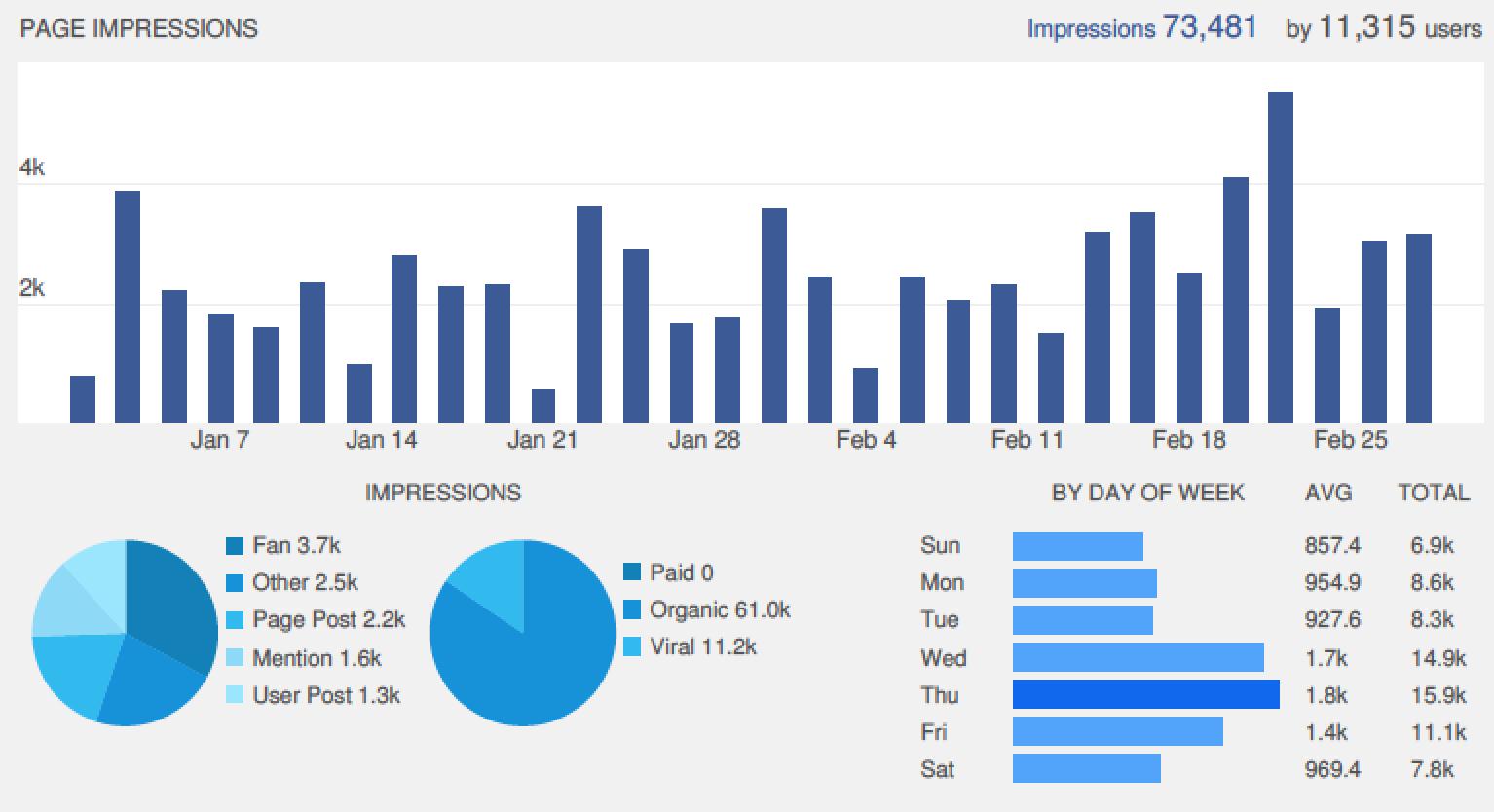
Lastly, we would again like to congratulate EAU and all the active Tweeters who contributed so much to the social media side of this year’s meeting. The final data from Symplur show huge activity which greatly expanded the reach and engagement of this meeting:
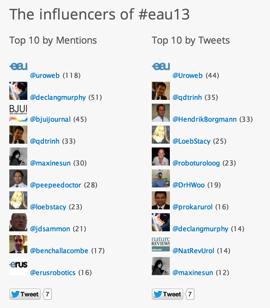
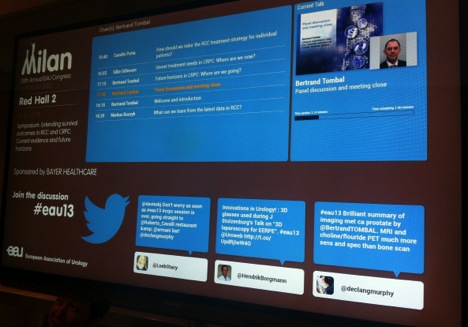
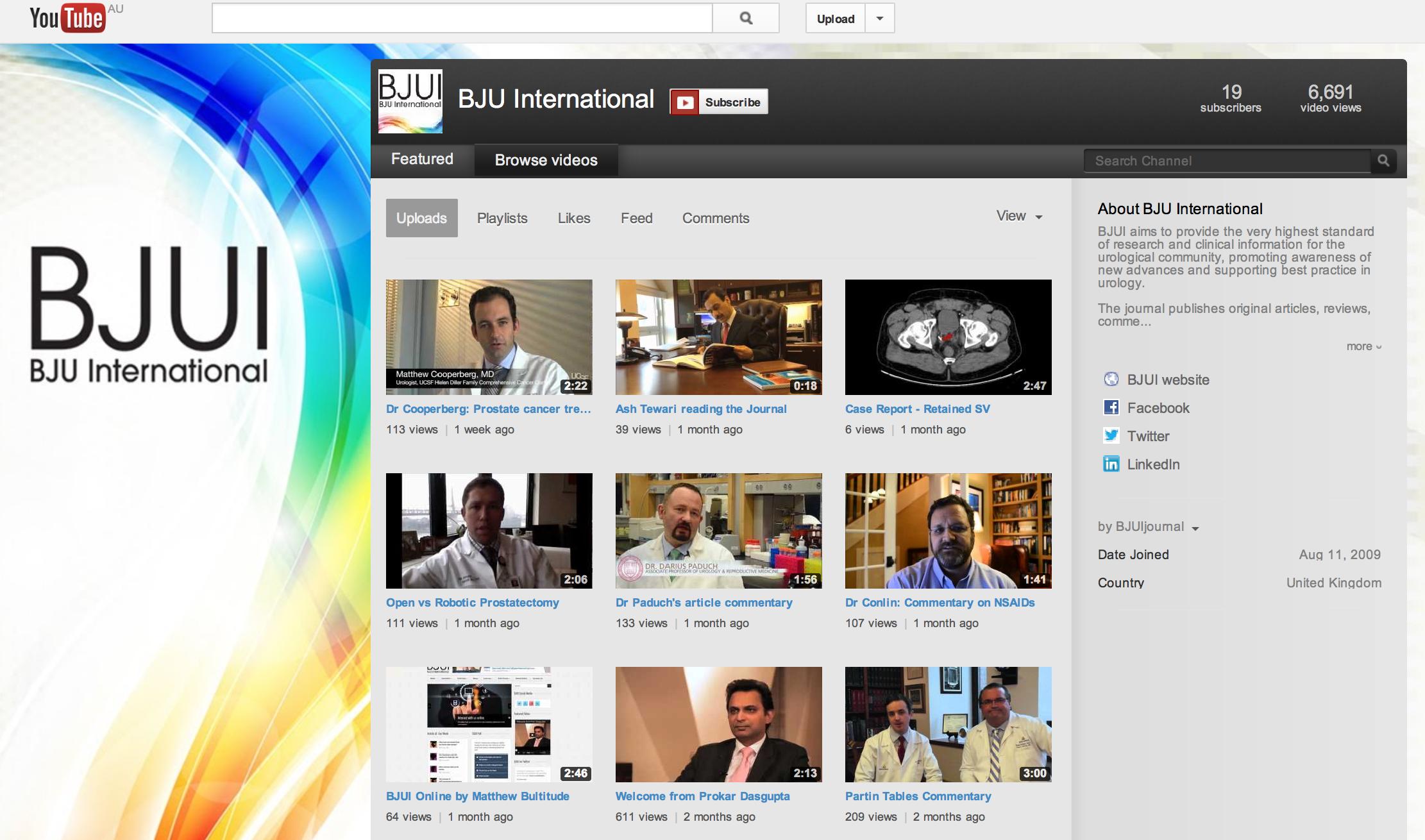
We are also very pleased that the BJUI team dominated the metrics for key influencers of #eau13 which reflects well on the strong social media strategy which we have put in place since January 2013. We were delighted to visit the busy EAU Communications back-office on the last day of the meeting to congratulate Communication Manager Evgenia “Zhenya” Starkova and her talented team who did a fantastic job running the Congress and EAU websites, twitter, facebook, video interviews etc and who we enjoyed interacting with through the week. Zhenya’s team kept tweeters engaged by awarding a “Tweet of the Day”:
EAU Official Tweets of the Day for the conference:
Friday – “Small renal masses, debate continues: surveillance vs biopsy vs partial vs radical neph. Individualised care is key.” @HamidAbboudi
Saturday – “#eau13 this is not just the European meeting now. It is the world meeting! What an event.”
@benchallacombe
Sunday – “It’s going to be a tough act for Stockholm to follow! Great congress so far! #eau13”@SJGore
Monday – “I suspect #eau13 will be remembered as 1st major urology meeting to do social media seriously. It’s been great fun!”@MattBultitude
So we look forward to EAU Annual Congress 2014 which takes place in Stockholm from 11-15th April 2014. We wish Scientific Chair Arnulf Stenzl and the team at EAU Central Office all the best with planning for next year’s meeting!
We will be back with more conference coverage from the Urological Society of Australia and New Zealand Annual Scientific Meeting that takes place in Melbourne next month (#usanz13).
Declan Murphy & Matt Bultitude
BJUI Associate Editors
Comments on this blog are now closed.