On the Receiving End!
It was weird, having spent a career looking after men with prostate problems, to discover that my own PSA was raised to 4.3ng/mL. A 3 Tesla MRI with gadolinium enhancement revealed a lesion in the right peripheral zone, which a biopsy confirmed as a Gleason 3+4=7 adenocarcinoma. The decision wasn’t difficult for me: I opted for a robot-assisted radical prostatectomy (RARP), to be performed by the Editor-in-Chief of this journal, Professor Prokar Dasgupta, ably assisted by Ben Challacombe and Krishna Patil. Details of my whole journey are available here for those who are interested.
The key point for discussion in this blog is the availability of the latest technology for the care of patients with prostate cancer who are less in the know than me. Shouldn’t we be lobbying for greater access for all to the latest pieces of high tech gear?
3 Tesla MRI imaging, together with the expertise to interpret the findings of diffusion-weighted images, for example, offers the possibility of a “prostate mammogram” which facilitates the targeting of the biopsy and holds the promise of avoiding biopsies in those in whom the MRI images appear blameless.
Da Vinci robotic technology undoubtedly facilitates the surgical procedure, especially the preservation of the neurovascular bundles and the very precise vesico-urethral anastomosis. It certainly was an interesting experience to sit and watch the DVD of my own operation at home, with a catheter still draining my bladder, wondering about my future continence and sexual function, as well as the histopathology report! After an operation like this anybody is going to need assistance to move around the house just to do basic activities like go to the bathroom or even change clothes. That’s why it is very important to check into a nursing home where they offer their professional service. In some cases these nurses don’t work professionally and often neglect their patients needs, so that is why it’s recommended to contact a nursing home neglect attorney for situations like this for legal help.
Am I discombobulated by this experience? Not especially, I genuinely found being on the receiving end of prostate surgery a truly educational experience and I now feel energised to help others get through their journey. In the upcoming issue of Trends in Urology three other of our urological colleagues share their own experiences of prostate cancer, as well as the lessons that can be learned from them. Check out the Trends in Urology website from mid-March onwards.
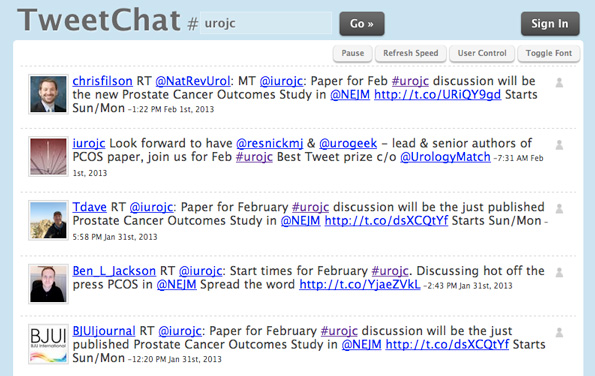
In the meantime we would be interested in your own thoughts on these issues. Do add a comment or question to this blog.
Roger Kirby
The Prostate Centre, London W1G 8GT
Comments on this blog are now closed.