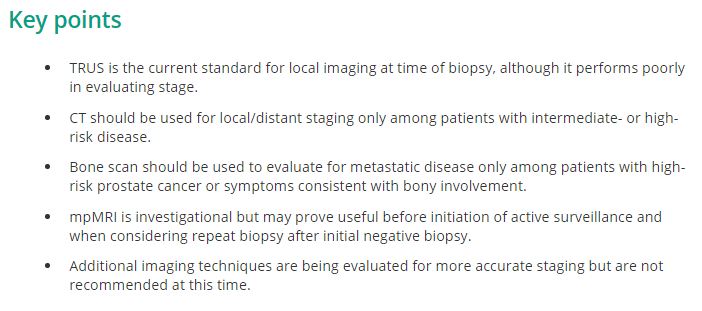
Guideline of Guidelines: Imaging of Localized Prostate Cancer
Introduction
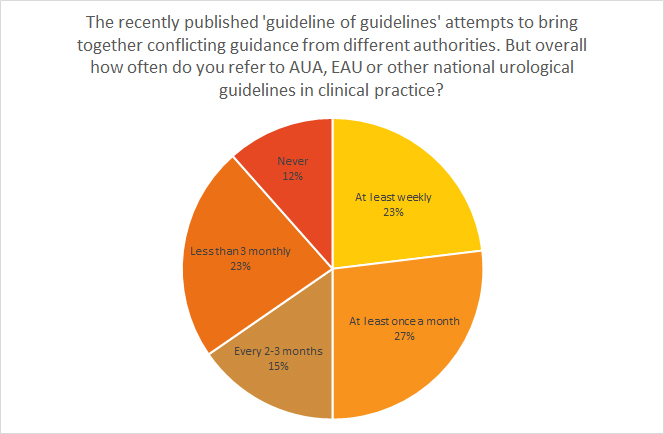
In the era before the widespread adoption of PSA screening for prostate cancer, most incident cases were already advanced stage. Because treatment options, such as surgery or radiation, are thought mainly to benefit patients with localised disease, prostate cancer imaging was necessary before treatment of almost all patients. However, in the PSA era >90% of incident cases are localised, making the need for routine imaging with CT, MRI, or bone scan obsolete [1]. Numerous studies show a relatively low rate of positive staging imaging in low- and intermediate-risk patients. Recognising these trends, several professional societies issued prostate cancer imaging guidelines in the mid-1990s in an effort to curb the overuse of imaging. However, despite these longstanding guidelines, a great number of patients undergo improper imaging [2]. Given how stubborn this problem has been to eradicate, there has been a renewed interest in finding ways to decrease unnecessary imaging, including a Physician Quality Reporting System (PQRS) quality measure and a highlighting of the problem in the ‘Choosing Wisely’ campaign [3-5]. In addition to the guidelines regarding the staging of incident prostate cancer, some groups have also presented guidelines on the use of imaging to follow men with advanced disease [6]. The purpose of the present article is to summarise the main points from multiple professional society guidelines on imaging in prostate cancer to help clarify when patients with prostate cancer should be imaged and with which modalities.