Editorial: Regaining continence after radical prostatectomy: RARP vs. ORP
Functional outcomes represent relevant criteria to evaluate the success of radical prostatectomy (RP) in the treatment of localised and locally advanced prostate cancer. Indeed, while the primary goal of RP remains the complete extirpation of the primary tumour, patients’ satisfaction can be negatively affected by urinary incontinence and/or erectile dysfunction after RP.
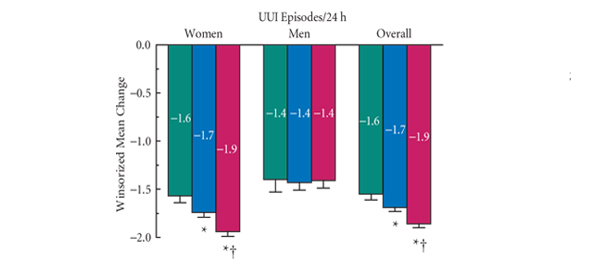
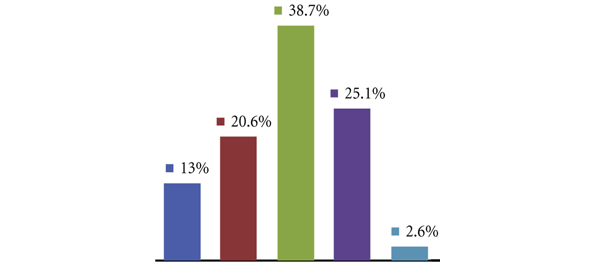
In this issue of BJUI, Geraerts et al. [1] evaluated urinary continence recovery and voiding symptoms in a well-conducted, single-centre, prospective non-randomised study comparing two contemporary series of patients who underwent either open retropubic RP (RRP) or robot-assisted RP (RARP) for clinically localised or locally advanced prostate cancer. Patients were assigned to each group according to their or their surgeon’s preference. High-risk prostate cancers were preferably treated with an open access to offer a more accurate extended lymphadenectomy. The study showed that the urinary continence recovery rate was significantly shorter in the RARP group than in the RRP group (16 vs 46 days; P = 0.008). Interestingly, the RA approach remained an independent predictor of time to urinary continence recovery on multivariable Cox regression analysis (P = 0.03; hazard ratio [HR] 1.52, 95% CI 1.03–2.26). Therefore, this study confirmed previously published results. In 2003, Tewari et al. [2] reported a shorter time to recovery of urinary continence in patients who underwent RARP (44 days) than those who received RRP (160 days). In 2008, Kim et al. [3] reported a median time to continence in RARP patients of 1.6 months, significantly lower than the 4.3 months in the RRP patients. Interestingly, Geraerts et al. [1] identified other independent predictors of time to continence, such as patient’s age >65 years (P = 0.02; HR 0.67, 95% CI 0.45–0.96) and the preoperative continence status (P = 0.004; HR 1.69, 95% CI 1.18–2.43). In all, 28% of patients who received RRP and 34% of those who underwent RARP were preoperatively defined as incontinent using a symptom-specific questionnaire [1]. These patients classifiable as ‘Cx’ according to the Survival, Continence and Potency (SCP) classification [4] represent a confounding population in the Geraerts et al. study who should be evaluated separately.
An interesting question is whether the reported difference in time to continence in favour of RARP is also significant from the clinical perspective. Urinary continence in patients who underwent RARP recovered 1 month early than those treated with traditional RRP. The King’s Health questionnaire seems to confirm a positive effect of this outcome on the patient’s quality of life (QoL). Indeed, there were better results in the RARP compared with RRP group at 1 and 3 months after RP. Moreover, at 12 months after RP, patients who underwent RRP were more physically limited (P = 0.01) and took more precautions to avoid urine loss (P = 0.01) than those who received a RARP [1]. These data seem to be in conflict with the reported overlapping 12-month urinary continence rates (96% in RRP and 97% in RARP group). Moreover, looking at the 12-month urinary continence rate, the Geraerts et al. study does not confirm the results of a recent cumulative analysis of available comparative studies showing a better 12-month urinary continence rate after RARP compared with RRP (odds ratio 1.53; P = 0.03) [1].
Interestingly, the 12-month urinary continence rate reported after RRP by Geraerts et al. is significantly higher (96%) than the values reported in the comparative studies included in the meta-analysis (88.7%) and in the most important and recent RRP non-comparative series (60–93%) [5]. This aspect appears to confirm the important role of surgeon experience. Indeed, in this Belgium series most of the open procedures were performed by an expert surgeon with experience of >3000 RRPs, and thus able to reach excellent functional outcomes for urinary continence recovery. In favour of robotic surgeons, we could consider that they were able to reach overlapping results after <200 cases.
In conclusion, the study published by Geraerts et al. [1] showed that modern RP in expert hands is able to achieve excellent results for urinary continence recovery regardless of the approach. However, pure and RA laparoscopy has pushed open surgeons to improve technical and postoperative aspects to achieve comparable outcomes. RARP can offer some advantages over traditional RRP, above all for the time to reach urinary continence. This advantage seems to have generated a better QoL profile in patients who underwent RARP at 12 months after RP.
However, the choice between the two techniques must be taken according to all the most relevant parameters including perioperative, functional (continence and potency) and oncological outcomes. Therefore, we strongly support the publication of clinical series or comparative studies reporting results according to the ‘trifecta’, ‘pentafecta’ or SCP systems [6].
Vincenzo Ficarra†°, Alessandro Iannetti* and Alexandre Mottrie†
†OLV Vattikuti Robotic Surgery Institute, Aalst, Belgium, °Department of Experimental and Clinical Medical Sciences – Urology Unit – School of Medicine, University of Udine, and *Department of Surgical, Oncologic and Gastrointestinal Sciences, Padua, Italy
References
- Geraerts I, Van Poppel H, Devoogdt N, Van Cleynenbreugel B, Joniau S, Van Kampen M. Prospective evaluation of urinary incontinence, voiding symptoms and quality of life after open and robot-assisted radical prostatectomy. BJU Int 2013; 112:936–943
- Tewari A, Srivasatava A, Menon M, Members of the VIP Team. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int 2003; 92: 205–210
- Kim SC, Song C, Kim W et al. Factors determining functional outcomes after radical prostatectomy: robot-assisted versus retropubic. Eur Urol 2011; 60: 413–419
- Ficarra V, Sooriakumaran P, Novara G et al. Systematic review of methods for reporting combined outcomes after radical prostatectomy and proposal of a novel system: the survival, continence, and potency (SCP) classification. Eur Urol 2012; 61:541–548
- Ficarra V, Novara G, Rosen RC et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012; 62: 405–417
- Ficarra V, Borghesi M, Suardi N et al. Long-term evaluation of survival, continence and potency (SCP) outcomes after robot-assisted radical prostatectomy (RARP). BJU Int 2013; 112: 338–345