Article of the Week: Silencing histone deacetylase 2 induces regression of fibrotic plaque in Peyronie’s disease
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Professor Ji-Kan Ryu discussing his paper.
If you only have time to read one article this week, it should be this one.
Silencing histone deacetylase 2 using small hairpin RNA induces regression of fibrotic plaque in a rat model of Peyronie’s disease
Ki-Dong Kwon, Min Ji Choi, Jin-Mi Park, Kang-Moon Song, Mi-Hye Kwon, Dulguun Batbold, Guo Nan Yin, Woo Jean Kim, Ji-Kan Ryu and Jun-Kyu Suh
National Research Center for Sexual Medicine and Department of Urology, Inha University School of Medicine, Incheon 400-711, Korea
OBJECTIVES
To examine the therapeutic effect of adenovirus encoding histone deacetylase 2 (HDAC2) small hairpin RNA (Ad-HDAC2 shRNA) in a rat model of Peyronie’s disease (PD) and to determine the mechanisms by which HDAC2 knockdown ameliorates fibrotic responses in primary fibroblasts derived from human PD plaque.
MATERIAL AND METHODS
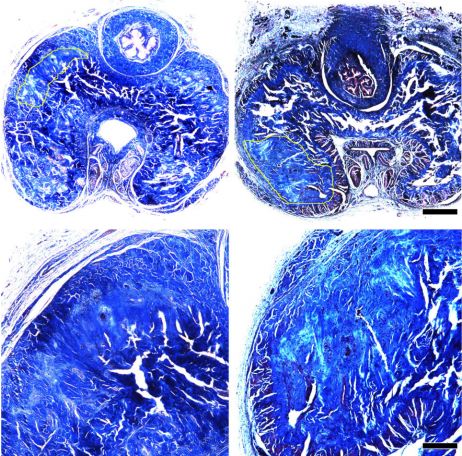
Rats were distributed into four groups (n = 6 per group): age-matched controls without treatment; rats in which PD has been induced (PD rats) without treatment; PD rats receiving a single injection of control adenovirus encoding scrambled small hairpin RNA (Ad-shRNA) (day 15; 1 × 108 pfu/0.1 mL phosphate-buffered saline [PBS]); and PD rats receiving a single injection of Ad-HDAC2 shRNA (day 15; 1 × 108 pfu/0.1 mL PBS) into the lesion. PD-like plaque was induced by repeated intratunical injections of 100 μL each of human fibrin and thrombin solutions on days 0 and 5. On day 30, the penis was harvested for histological examination. Fibroblasts isolated from human PD plaque were pretreated with HDAC2 small interfering (si)RNA (100 pmoL) and then stimulated with transforming growth factor (TGF)-β1 (10 ng/mL) to determine hydroxyproline levels, procollagen mRNA, apoptosis and protein expression of poly(ADP-ribose) polymerase 1 (PARP1) and cyclin D1.
RESULTS
We observed that Ad-HDAC2 shRNA decreased inflammatory cell infiltration, reduced transnuclear expression of phospho-Smad3 and regressed fibrotic plaque of the tunica albuginea in PD rats in vivo. siRNA-mediated silencing of HDAC2 significantly decreased the TGF-β1-induced transdifferentiation of fibroblasts into myofibroblasts and collagen production, and induced apoptosis by downregulating the expression of PARP1, and decreased the expression of cyclin D1 (a positive cell-cycle regulator) in primary cultured fibroblasts derived from human PD plaque in vitro.
CONCLUSION
Specific inhibition of HDAC2 with RNA interference may represent a novel targeted therapy for PD.