Editorial: The age old question: who benefits from prostate cancer treatment?
Widespread PSA-based screening has dramatically altered the profile of newly diagnosed prostate cancer in many countries. Although screening effectively decreases the rates of metastatic disease and prostate cancer death [1], the increasing proportion of low-risk disease necessitates a critical assessment of the need for aggressive therapy.
Active surveillance and watchful waiting are potential alternatives to delay or avoid the need for treatment in carefully selected patients. The key issue is determining which patients are appropriate for conservative management. Although these approaches are often targeted toward elderly men, such men are more likely to be diagnosed with high-risk disease. A recent study by Scosyrev et al. [2] raised concern about excess prostate cancer mortality attributable to under-treatment in the elderly.
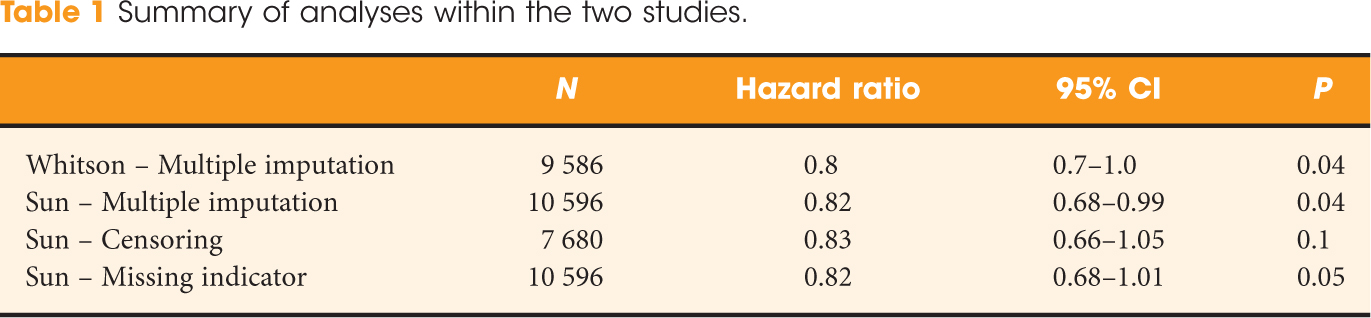
Overall, there is very little Level 1 evidence to guide prostate cancer treatment selection. One such trial, the Swedish Prostate Cancer Group 4 (SPCG-4), showed that radical prostatectomy significantly improved survival compared with watchful waiting [3]; however, that study examined a primarily clinically detected population from the 1990s. Subsequently, the Prostate Cancer Intervention versus Observation Trial (PIVOT) randomized US male veterans diagnosed with prostate cancer from 1994 to 2002 to radical prostatectomy vs observation [4]. At 10 years, they reported no significant difference in overall survival between the two arms in the intent-to-treat analysis (hazard ratio 0.88; 95% CI 0.71–1.08, P = 0.22). However, that study was smaller than anticipated owing to difficulty with recruitment and there was a high rate of crossovers between the intervention and observation arms. Per-protocol analysis was not reported for PIVOT and the prostate cancer landscape has continued to change in the past decade, raising unanswered questions over what the results would be if we compared contemporary men who were actually treated to those who were not.
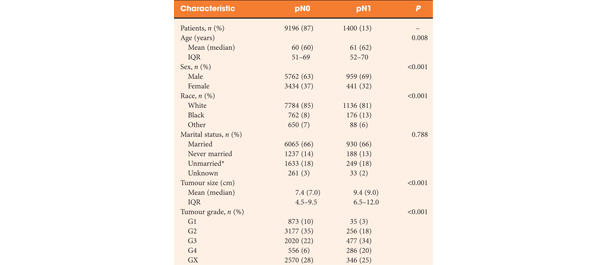
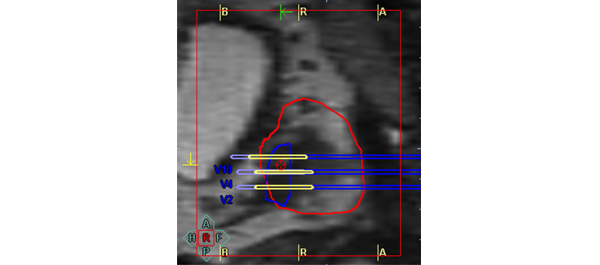
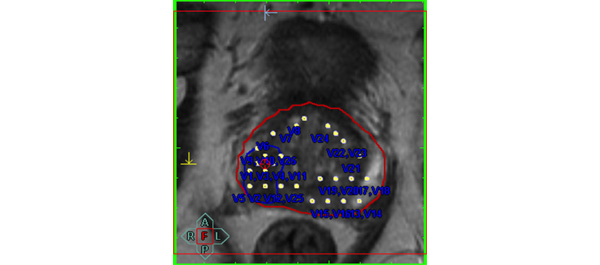
This is the knowledge gap addressed by Aizer et al. [5] who used Surveillance, Epidemiology and End Results (SEER) data for 27 969 US men diagnosed with low-risk prostate cancer from 2004 to 2007. Overall, 67.1% of these men received radical prostatectomy or radiation therapy, while >30% underwent active surveillance or watchful waiting. Using competing risks regression, they showed that both age and non-curative treatment were associated with a significantly higher short-term prostate cancer-specific mortality. These results should be interpreted with caution, however, since they comprise observational data with great potential for confounding. Interestingly, at a short median follow-up of only 2.75 years, 5.4% of these men with presumed low-risk disease died from prostate cancer. Recently, there has been debate over whether Gleason 6 disease should really be considered a cancer [6], but these data highlight the limitations of current clinical staging, such that even presumed low-risk disease may be understaged. The authors suggest that use of a more extended biopsy scheme before active surveillance might reduce the risk of early progression due to undersampling. MRI represents another potential non-invasive treatment method to improve clinical staging and patient selection for active surveillance in the future [7].
Stacy Loeb
Department of Urology, New York University, New York, NY, USA
References
- Schroder FH, Hugosson J, Roobol MJ et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012; 366: 981–990
- Scosyrev E, Messing EM, Mohile S et al. Prostate cancer in the elderly: frequency of advanced disease at presentation and disease-specific mortality. Cancer 2012; 118: 3062–3070
- Bill-Axelson A, Holmberg L, Ruutu M et al. Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med 2011; 364: 1708–1717
- Wilt TJ, Brawer MK, Jones KM et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med 2012;367: 203–212
- Aizer AA, Chen MH, Hattangadi J, D’Amico AV. Initial management of prostate-specific-antigen-detected, low-risk prostate cancer and the risk of death from prostate cancer. BJU Int 2014; 113: 43–50
- Carter HB, Partin AW, Walsh PC et al. Gleason score 6 adenocarcinoma: should it be labeled as cancer? J Clin Oncol 2012; 30:4294–4296
- Vargas HA, Akin O, Afaq A et al. Magnetic Resonance Imaging for Predicting Prostate Biopsy Findings in Patients Considered for Active Surveillance of Clinically Low Risk Prostate Cancer. J Urol 2012; 188: 1732–1738