Video: Move over fluoroscopy: ultrasound-guided PCNL is just as good
Percutaneous nephrolithotomy guided solely by ultrasonography: a 5-year study of >700 cases
Song Yan, Fei Xiang and Song Yongsheng
Division of Urology, Sheng Jing Hospital, China Medical University, Shenyang, China
OBJECTIVE
• To evaluate the safety and efficacy of percutaneous nephrolithotomy (PCNL) solely guided by ultrasonography (US).
PATIENTS AND METHODS
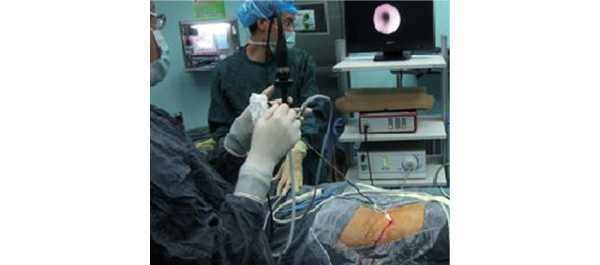
• From May 2007 to July 2012, 705 24-F-tract PCNL procedures were performed (679 patients, of whom 26 had bilateral stones).
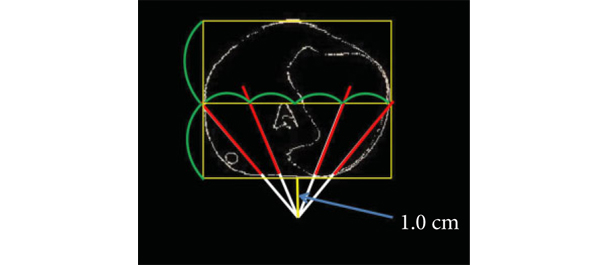
• Calyceal puncture and dilatation were performed under US guidance in all cases.
• The procedure was evaluated for access success, length of postoperative hospital stay, complications (modified Clavien system), stone clearance and the need for auxiliary treatments.
RESULTS
• The mean (sd) operating time was 66 (25) min, with a mean (sd) postoperative hospital stay of 3.98 (1.34) days.
• The patients experienced a mean (sd) haemoglobin level decrease of 2.24 (2.02) g/day and the overall stone-free rate at 4 weeks after surgery was 92.6% in patients with a single calculus and 82.9% in patients with staghorn or multiple calculi.
• Auxiliary treatments, including shockwave lithotripsy in 52 patients, re-PCNL in 41 patients and ureteroscopy in 18 patients, were performed 1 week after the primary procedure in 111 (15.7%) cases for residual stones >4 mm in size.
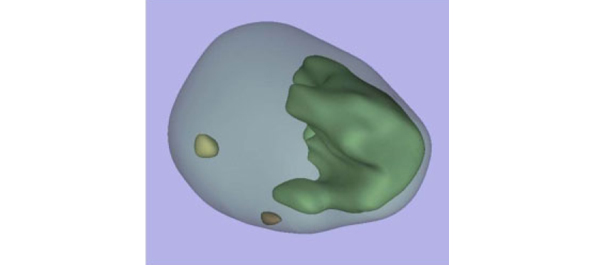
• The sensitivities of intra-operative US-guidance and flexible nephroscopy for detecting significant residual stones and clinically insignificant residual fragments were 95.3 and 89.1%, respectively.
• There were 94 grade 1 (13.3%), 17 grade 2 (2.4%), and two grade 3 (0.3%) complications, but there were no grade 4 or 5 complications.
CONCLUSION
• Total US-guided PCNL is safe and convenient, and may be performed without any major complications and with the advantage of preventing radiation hazards and damage to adjacent organs.