Posts
IP2 – ATLANTA is launched!
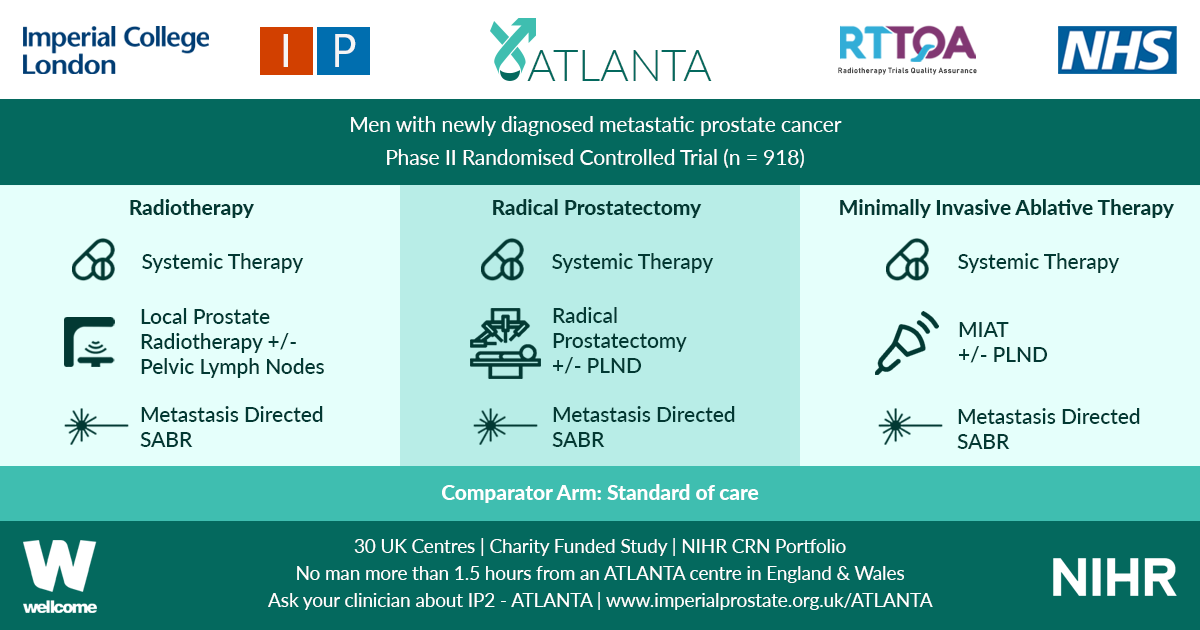
IP2 – ATLANTA is launched! ATLANTA is a phase II randomised controlled trial that will explore sequential multi-modal treatment using systemic therapy, local physical cytoreduction and metastasis directed therapy in men with newly diagnosed metastatic prostate cancer against a comparator of standard of care alone.
All men with new histologically diagnosed hormone sensitive metastatic prostate cancer, within three months of commencing androgen deprivation therapy (ADT), and of performance status 0 to 2 are eligible. No upper limit on metastatic burden will apply, although men must be fit to undergo all trial interventions at point of randomisation.
Men will be randomised to: Control (Standard of Care) OR Intervention 1 (Minimally Invasive Ablative Therapy [MIAT] +/- pelvic lymph node dissection [PLND]) OR Intervention 2 (Local Radiotherapy +/- Lymph Nodes OR Radical Prostatectomy +/- PLND). Randomisation stratified by metastatic burden (CHAARTED definition), intent to treat pelvic lymph nodes, intent to treat metastasis and intent to commence chemotherapy.
Systemic therapy in all arms includes ADT +/- Docetaxel. Radical prostatectomy will be with or without PLND. Local radiotherapy will be 60Gy/20Fr OR 74-78Gy in 2Gy per fraction over a minimum of 27 days, with or without simultaneous nodal radiotherapy. MIAT will be cryotherapy or focal HIFU. Men in both intervention arms will be eligible for metastasis directed therapy in the form of stereotactic ablative radiation (SABR) or surgery.
Men will be recruited over a two year period and followed up for a minimum of two years. Primary outcome will be progression free survival (PFS). ATLANTA is commencing in 17 UK trial centres with a target recruitment of 80 patients in the internal pilot, rising to 918 patients in full phase across 30 UK trial centres from November 2019.
ATLANTA is entirely charity funded (Wellcome Trust) and available on the NIHR CRN portfolio. Follow-up trial visits are not in excess of routine practice and extra burden is minimal. If you would like to join the main phase of ATLANTA as a site, please contact Mr Martin J. Connor ([email protected]) www.imperialprostate.org.uk/ATLANTA.
Prof. Hashim U. Ahmed (ATLANTA PI & CI),
Mr. Martin J. Connor (ATLANTA Doctoral Clinical Research Fellow)
Mr. Taimur T. Shah (Urology SpR & Research Fellow)
ATLANTA Surgeons Board: Mr Mathias Winkler, Mr Tim Dudderidge, Prof. Chris Eden, Mr Paul Cathcart, Prof. Naeem Soomro, Mr Adel Makar
ATLANTA Radiotherapy Board: Prof. John Staffurth, Dr. Alison Falconer, Dr. Stephen Mangar, Dr Olivia Naismith, RTTQA team
ATLANTA MIAT Board: Prof. Hashim U. Ahmed, Mr Stuart McCracken, Mr Raj Nigam, Mr Tim Dudderidge, Prof Iqbal Shergill
ATLANTA SABR Board: Dr Vincent Khoo, RTTQA team
ATLANTA Medical Oncologists: Dr. Naveed Sarwar, Dr Michael Gonzalez
ATLANTA Trial Sites: Imperial College Healthcare NHS Trust, The Royal Marsden Hospital, Guy’s & St Thomas’ NHS Foundation Trust, London North West Healthcare NHS Trust, Royal Surrey County (Guildford) Hospital, University Hospital Southampton, Clatterbridge Cancer Centre & Arrowe Park Hospital, Newcastle Freeman Hospital, King’s Lynn (Cambridge), Norfolk & Norwich (Cambridge), Sunderland Royal Hospital, Frimley Park Hospital, Royal Devon and Exeter Hospital, Wrexham Park Hospital, West Middlesex University Hospital, Royal United Hospital Bath, Betsi Calderwar Health Board, Lister Hospital, Hampshire (Basingstoke) Hospitals, University Hospital Coventry, Worcestershire Royal Hospital.
Trial Sponsor: Imperial College London
Trial Funder: Wellcome Trust
ClinicalTrials.gov Identifier: NCT03763253
Article of the week: Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: subgroup analysis from a blinded randomized trial
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: subgroup analysis from a blinded randomized trial
Abstract
Objective
To test the hypothesis that benign prostatic hyperplasia (BPH) robotic surgery with aquablation would have a more pronounced benefit in certain patient subgroups, such as men with more challenging anatomies (e.g. large prostates, large middle lobes) and men with moderate BPH.
Methods
We conducted prespecified and post hoc exploratory subgroup analyses from a double‐blind, multicentre prospective randomized controlled trial that compared transurethral resection of the prostate (TURP) using either standard electrocautery vs surgery using robotic waterjet (aquablation) to determine whether certain baseline factors predicted more marked responses after aquablation as compared with TURP. The primary efficacy endpoint was reduction in International Prostate Symptom Score (IPSS) at 6 months. The primary safety endpoint was the occurrence of Clavien–Dindo persistent grade 1 or grade ≥2 surgical complications.
Results
For men with larger prostates (50–80 g), the mean IPSS reduction was four points greater after aquablation than after TURP (P = 0.001), a larger difference than the overall result (1.8 points; P = 0.135). Similarly, the primary safety endpoint difference (20% vs 46% [26% difference]; P = 0.008) was greater for men with large prostate compared with the overall result (26% vs 42% [16% difference]; P = 0.015). Postoperative anejaculation was also less common after aquablation compared with TURP in sexually active men with large prostates (2% vs 41%; P < 0.001) vs the overall results (10% vs 36%; P < 0.001). Exploratory analysis showed larger IPSS changes after aquablation in men with enlarged middle lobes, men with severe middle lobe obstruction, men with a low baseline maximum urinary flow rate, and men with elevated (>100) post‐void residual urine volume.
Conclusions
In men with moderate‐to‐severe lower urinary tract symptoms attributable to BPH and larger, more complex prostates, aquablation was associated with both superior symptom score improvements and a superior safety profile, with a significantly lower rate of postoperative anejaculation. The standardized, robotically executed, surgical approach with aquablation may overcome the increased outcome variability in more complex anatomy, resulting in superior symptom score reduction.
Editorial: A novel robotic procedure for bladder outlet obstruction
We have become used to talking about robotic surgery in urology when we really mean robot‐assisted surgery. The novel aquablation procedure (AquaBeam®) for bladder outlet obstruction (BOO) described by Plante et al. [1] is executed by a robotically controlled waterjet system, conducting a pre‐planned image‐guided resection once the radiological parameters have been entered into the system. This is performed under real‐time ultrasonography guidance. It will deliver a standardized way of carrying out the surgery and will, to a large extent, take away the surgical learning curve whilst introducing a new imaging learning curve.
The present study [1] is an analysis of pre‐planned and exploratory subsets of patients from the WATER study [2], and confirms data from earlier studies [3,4]. The study suggests that, compared with TURP, aquablation is particularly effective in improving both LUTS and bother in the medium‐sized to larger prostate (50–80 mL) and in potentially more challenging prostates such as those with large middle lobes or middle lobe obstruction (judged at pre‐procedure cystoscopy).
It is suggested that the ability to map the resection plane surgically may enable the preservation of key anatomical landmarks and preserve normal sexual function. In this study, anejaculation occurred in only 2% of patients with larger prostates (>50 mL) in the aquablation group compared with 41% of comparable patients undergoing TURP (P < 0.001). The rate of anejaculation however appeared relatively higher in the overall aquablation group, at 10%, compared with 36% in the overall TURP group (P < 0.001). A prostate volume between 30 and 80 mL was an inclusion criterion for the WATER study. This procedure therefore appears to give the best possible rate of anejaculation in a resective surgical intervention in patients with a larger prostate and may have less advantage in patients with a smaller prostate.
Interestingly, the relative overall symptom relief advantage of aquablation over TURP was also not proven in men with smaller prostates; TURP may be equally effective at removing obstructing tissue in smaller as compared to larger prostates. It is not yet clear whether aquablation would not be recommended for prostates below a certain size. In the more recent WATER II study in 101 men with a mean prostate volume of 107 mL, aquablation was also shown to be feasible and safe in men with large prostates (80–150 mL) [5].
There will always be a possible downside to novel treatments and this may relate to poor radiological data entry which may, in turn, lead to sphincter damage, although this has not been an issue in the carefully controlled studies to date. There are also reports of troublesome postoperative bleeding in some cases, although haemostasis can be effectively achieved via a catheter balloon tamponade and traction device or by electrocautery [5,6].
Unlike most other surgical treatments for BOO, the resection times for aquablation are almost independent of prostate volume, although the overall operating time is similar to that of TURP, with the majority of the time being spent in the set up and image planning.
The principal study (WATER) [2] on which this sub‐analysis by Plante et al. is based is an example of a high‐quality randomized controlled trial but still represents data on only 116 patients undergoing aquablation and 65 undergoing TURP; therefore, more randomized controlled trial data and long‐term effectiveness studies are clearly needed. Formal urodynamic studies and trials in patients with even larger prostates would also be appropriate. In addition, there are still few published data on the cost‐effectiveness of aquablation, although it is likely to be in the range of higher‐cost laser ablation therapies.
With better radiology and machine learning or artificial intelligence, this technique may lead to truly standardized BOO surgery with more complete resection and may thereby reduce outcome variability.
References
- , , et al. Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: subgroup analysis from a blinded randomized trial. BJU Int 2019; 123: 651– 60
- , , et al. WATER: a double‐blind, randomized, controlled trial of Aquablation® vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol 2018; 199: 1252– 61
- , , et al. Aquablation ‐ image‐guided robot‐assisted waterjet ablation of the prostate: initial clinical experience. BJU Int 2016; 117: 923– 9
- , , . Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1‐year results. J Urol 2017; 197: 1565– 72
- , , et al. WATER II (80‐150 mL) procedural outcomes. BJU Int 2019;123: 106– 12
- , , . How I do it: balloon tamponade of prostatic fossa following Aquablation. Can J Urol 2017; 24: 8937– 40
Encouraging future urologists: BAUS Section of Trainees (BSoT) goes to ASiT Conference
The Association of Surgeons in Training (ASiT) is a trainee-led, pan-specialty, independent body that aims to promote the highest standards of surgical training. The highlight of their calendar is the ASiT Conference, this year held at the ICC Belfast from 22nd to 24th March 2019. It attracted over 700 delegates of all grades.
ASiT invites representatives of all surgical specialty groups to be part of their council. It is a reciprocal relationship as many surgical training issues affect us all and together we have a great influence. Urology’s BAUS Section of Trainees ‘BSoT’ (formerly SURG) Representative, Clare Jelley (ST5, Oxford Deanery), has done an incredible job over the last 3 years and it is these shoes that I now attempt to fill as the new BSoT/ASiT Rep.
Are you a urologist and desire to find a good job offer? Check out vacancies on Jooble.
The ASiT Conference weekend included pre-conference courses run by surgical specialty groups, plenary lectures with notable speakers, breakout sessions and an impressive exhibition hall. Unsurprisingly the plenary session on curricula, credentialing and regulation was full; Charlie Massey and Prof Colin Melville (GMC) were put under fierce questioning by the ASiT Committee and the audience. The plenary talks also included a range of topics: innovation, leadership, burnout, fatigue and overcoming adversity. The latter was poignantly given by John Peter, RAF pilot and POW in Iraq (pictured).
The scientific programme included research and audit project presentations. Successful abstract submissions were invited for poster presentation (grouped and marked by specialty) and the highest scoring, prize-worthy abstracts were invited for oral presentation. Accepted abstracts are published in the British Journal of Surgery. There were also social events including a 5km charity run, welcome drinks and the inaugural black-tie Gala Dinner held at the stunning Belfast City Hall.
Clare and I flew the flag for Urology during the conference! The pre-conference course ‘Basic Urology Skills’ was full; we taught 16 very keen delegates interested in a career in urology from all over the UK (pictured). We included practical stations to teach skills such as: cystoscopy, ureteric stenting, scrotal exploration (using medical meat), circumcision and supra-pubic catheter insertion. We are very grateful for reps from Cook, Stryker and Coloplast for providing the equipment and to our urological trainee faculty which included Mr Trevor Thompson, urological consultant and Head of the School of Surgery in Belfast, UK.
The ‘Specialty Fair’ was another opportunity to showcase urology (and promote it as the best career choice!). The room was packed. Delegates met speciality representatives and trainees, enabling conversations and questions about their surgical specialty in an informal manner. Special thanks to urology registrars Tharani Mahesan and Katie Chan who helped spread the positive message (pictured).
The abstract p resentations were of a high standard; there were over 50 urology-themed posters showcased. Of particular note there were at least 4 oral presentations reflecting projects within urology – including IDENTIFY preliminary results presented by Tara Sibartie on behalf of all the collaborators, which won the Society of Academic and Research Surgery (SARS) prize. Another urological highlight was the Edinburgh Surgical Sciences Qualification prize being awarded to Katie Chan for her presentation of the #DontPayToStay campaign. This Freedom of Information request exposed that 18% of English hospitals charge for non-resident on call accommodation at a median rate of £25/night. i.e. trainees are left with a financial burden in order to maintain a safe emergency practice. By highlighting this issue and gaining support from ASiT and the Junior Doctors Committee it is hoped that these charges can conclusively be removed during the renegotiation of the junior doctor contract. Katie also brought along the youngest Conference delegate, baby Orla, who enjoyed the use of the ASiT crèche (free of charge!).
resentations were of a high standard; there were over 50 urology-themed posters showcased. Of particular note there were at least 4 oral presentations reflecting projects within urology – including IDENTIFY preliminary results presented by Tara Sibartie on behalf of all the collaborators, which won the Society of Academic and Research Surgery (SARS) prize. Another urological highlight was the Edinburgh Surgical Sciences Qualification prize being awarded to Katie Chan for her presentation of the #DontPayToStay campaign. This Freedom of Information request exposed that 18% of English hospitals charge for non-resident on call accommodation at a median rate of £25/night. i.e. trainees are left with a financial burden in order to maintain a safe emergency practice. By highlighting this issue and gaining support from ASiT and the Junior Doctors Committee it is hoped that these charges can conclusively be removed during the renegotiation of the junior doctor contract. Katie also brought along the youngest Conference delegate, baby Orla, who enjoyed the use of the ASiT crèche (free of charge!).
BSoT is committed to representing current urology trainees but also to inspire and mentor medical students, foundation and core trainees who may be interested in a career in urology. Therefore it was a privilege to be able to represent the newly rejuvenated BSoT; perhaps even encouraging some future urologists!
Overall it was an exciting and interesting weekend; ASiT Conference 2020 will be held at the ICC Birmingham from 6th to 8th March; it promises to be bigger and better than ever and BSoT will be there! I’d thoroughly recommend all those interested in a career in surgery (and urology) to submit their projects, attend and get involved with ASiT. BSoT will also be organising events for those interested in a career in urology – so watch this space!
by Sophie Rintoul-Hoad, ST5 Urology trainee in South London Deanery and recently elected ASiT representative for BAUS Section of Trainees Committee (BSoT).
Acknowledgements: Clare Jelley and Luke Forster (BSoT President)
BAUS/BJUI/USANZ Joint Session AUA 2019
British Association of Urological Surgeons/BJU International/Urological Society of Australia and New Zealand (BAUS/BJUI/USANZ) Joint Session AUA 2019
Sunday, May 5th 2:00 – 5.00 PM. McCormick Place Convention Center South Building – Room S102 BC
|
Registries /Smart Data /Complications – CHAIR: Duncan Summerton
|
|
| 1400-1420 | Alan Partin
A contemporary look at biomarkers for diagnosis of Prostate Cancer |
| 1420-1440 | Chris Harding (BJUI sponsored BAUS lecture)
The Mesh Story – lessons learned and future plans |
| 1440-1500 | Nick Watkin
PROMs in Urology |
| 1500-1520 | Stephen Mark
Big Data and Urology – a pilot trial in New Zealand |
| 1520-1540 | Afternoon tea |
|
Education /Training /Innovation – CHAIR: Prokar Dasgupta
|
|
| 1540-1600 | Andrew Hung (BJUI sponsored lecture)
The emerging role of Artificial Intelligence in Surgical Science |
| 1600-1620 | Jonathan Kam
Zero learning curve Percutaneous Nephrolithotomy Access – Prone endoscopic combined intrarenal surgery and multimedia training aid to teach urology trainees |
| 1620-1640 | Madhu Koya (BJUI sponsored USANZ lecture)
Cx bladder reduces flexible cystoscopy in haematura and superficial TCC |
| 1640-1700 | Kamran Ahmad
Innovation in healthcare systems |
| 1700-1705 | BJUI Coffey-Krane Award for trainees based in The Americas presented by Prokar Dasgupta |
| 1700-1900 | BJUI Reception |
Article of the week: A clinical prediction tool to determine the need for concurrent systematic sampling at the time of MRI‐guided biopsy
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
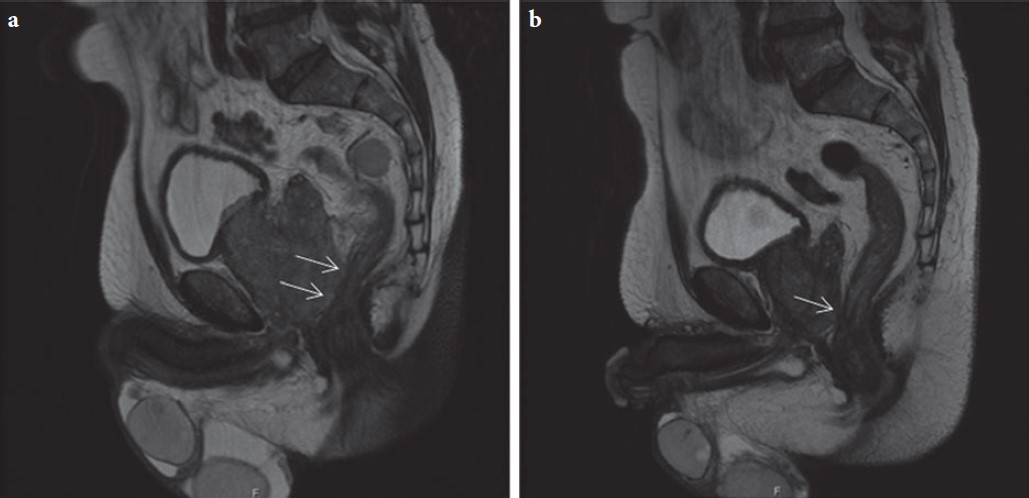
A clinical prediction tool to determine the need for concurrent systematic sampling at the time of magnetic resonance imaging‐guided biopsy
Abstract
Objective
To develop a clinical prediction tool that characterises the risk of missing significant prostate cancer by omitting systematic biopsy in men undergoing transrectal ultrasonography/magnetic resonance imaging (TRUS/MRI)‐fusion‐guided biopsy.
Patients and methods
A consecutive sample of men undergoing TRUS/MRI‐fusion‐guided biopsy with the UroNav® system (Invivo International, Best, The Netherlands) who also underwent concurrent systematic biopsy was included. By comparing the grade of cancer diagnosed on targeted and systematic biopsy cores, we identified cases where clinically significant disease (Gleason score ≥3+4) was only found on systematic and not targeted cores. Multivariable logistic regression analyses were used to identify predictive factors for finding significant cancer on systematic cores only. We then used these data to develop a nomogram and evaluated its utility using decision curve analysis.
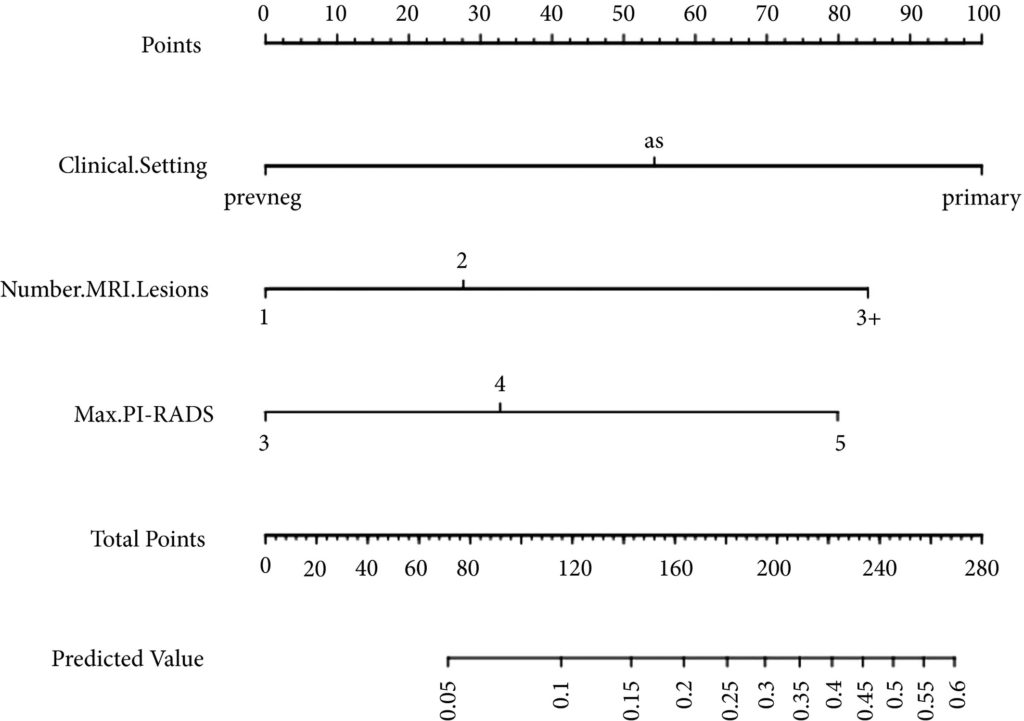
Fig 1. Nomogram for predicting the diagnosis of clinically significant on systematic biopsy only and missed on targeted biopsy.
Results
Of the 398 men undergoing TRUS/MRI‐fusion‐guided biopsy in our study, there were 46 (11.6%) cases in which clinically significant cancer was missed on targeted biopsy and detected on systematic biopsy. The clinical setting, number of MRI lesions identified, and the highest Prostate Imaging‐Reporting and Data System (PI‐RADS) score of the lesions, were all found to be predictors of this. Our model had a good discriminative ability (concordance index = 0.70). The results from our decision curve analysis show that this model provides a higher net clinical benefit than either biopsying all men or omitting biopsy in all patients when the threshold probability is <30%.
Conclusion
We found that omitting concurrent systematic biopsy in men undergoing TRUS/MRI‐fusion‐guided biopsy would miss significant disease in more than one in 10 patients. We propose a prediction model with good discriminative ability that can be used to improve patient selection for performing concurrent systematic biopsy in order to minimise the number of missed significant cancers. It is important that our model is validated in external cohorts before being employed in routine clinical practice.
Editorial: Can systematic biopsy be safely avoided at the time of MRI/ultrasonography fusion biopsy?
In clinical practice, the need for maximising prostate cancer detection is often balanced against the theoretical risks of infection, bleeding, and pain associated with taking additional cores. In this novel study, Sathianathen et al. [1] provide a tool for measuring the oncological benefit of including concurrent systematic biopsy (SB) at the time of MRI‐guided targeted biopsy (TB). There were several key findings: (i) Amongst patients undergoing MRI‐guided biopsy (all biopsy settings), 11.6% were found to have significant cancers detected by SB alone; (ii) Amongst patients who had clinically significant cancers detected by SB alone, 52.2% were sampled within sextants outside the targeted regions of interest; (iii) According to the proposed nomogram, patients with prior negative biopsies, fewer MRI lesions, and lower Prostate Imaging‐Reporting and Data System (PI‐RADS) scores were at the lowest risk of missing significant cancer when SB was omitted.
Based on the present study, biopsy setting appears to be a key factor for deciding whether to omit SB. In the subset of patients undergoing primary biopsy, the authors found that 18.5% of cancers were detected by SB alone. These results are consistent with those of the MRI‐FIRST trial, which showed 14% of cancers were detected by SB only, 20% by TB only, and 66% by combining both techniques [2]. MRI‐FIRST concluded that in the primary biopsy setting, there was no difference between SB and TB in detection of clinically significant prostate cancer, although combining both techniques provided the highest detection rate.
Prior negative biopsy cohorts are generally at lower risk of harbouring significant cancer, as many cancers have already been ‘selected out’ by initial biopsies. In this setting, TB plays an important role in sampling tumour foci in difficult‐to‐reach regions of the prostate (e.g., anterior and apical) [3]. According to the authors’ nomogram, prior negative biopsy patients were least likely to benefit from concurrent SB. While the authors suggest a paradigm of selectively omitting SB, some authors have proposed omitting both TB and SB altogether in select patients. A previously reported multi‐institutional nomogram can be used to predict benign pathology after MRI‐guided biopsy, which can help reduce the number of unnecessary biopsies after MRI in the prior negative biopsy setting [4]. This clinical tool was further externally validated and optimised by Bjurlin et al. [5].
The ‘active surveillance (AS)’ setting typically refers to a confirmatory MRI‐guided biopsy in men with Grade Group 1 prostate cancer prior to enrollment in AS. Recently, the presence of cribriform morphology in Grade Group 2 patients was confirmed to be a key poor prognostic feature that would exclude patients from AS [6]. The present study, however, did not account for different Gleason pattern 4 morphologies in their analysis, as ‘significant cancer’ was defined by Grade Group alone. Studies by independent groups have found that TB combined with SB was more accurate than either modality alone for detecting cribriform at the time of MRI‐guided biopsy [7, 8]. Therefore, concurrent SB is required to properly sample cribriform cancers in patients who are considering AS.
In this study, Sathianathen et al. [1] provide clinicians with a clinical tool for quantifying the added oncological value of concurrent SB. However, concurrent SB is probably prudent for most patients, particularly for those considering AS or focal therapy for which accurate determination of whole gland grade, cancer volume, and cribriform status are essential. As reducing the number of cores has not yet been shown to reduce biopsy‐related complications, are we willing to suboptimise cancer sampling without proven compensation?
by Matthew Truong
References
- , , et al. A clinical prediction tool to determine the need for concurrent systematic sampling at the time of magnetic resonance imaging‐guided biopsy. BJU 2019; 123: 612– 7
- , , et al. In patients with a previous negative prostate biopsy and a suspicious lesion on magnetic resonance imaging, is a 12‐core biopsy still necessary in addition to a targeted biopsy? BJU Int 2015; 115: 562– 70
- , , et al. Multi‐institutional nomogram predicting benign prostate pathology on magnetic resonance/ultrasound fusion biopsy in men with a prior negative 12‐core systematic biopsy. Cancer 2018; 124: 278– 85
- , , et al. Predicting benign prostate pathology on magnetic resonance imaging/ultrasound fusion biopsy in men with a prior negative 12‐core systematic biopsy: external validation of a prognostic nomogram. Eur Urol Focus 2018. [Epub ahead of print] https://doi.org/10.1016/j.euf.2018.05.005
- , , et al. Presence of invasive cribriform or intraductal growth at biopsy outperforms percentage grade 4 in predicting outcome of Gleason score 3+4=7 prostate cancer. Mod Pathol 2017; 30: 1126– 32
- , , et al. A comprehensive analysis of cribriform morphology on magnetic resonance imaging/ultrasound fusion biopsy correlated with radical prostatectomy specimens. J Urol 2018; 199: 106– 13
- , , et al. Role of magnetic resonance imaging targeted biopsy in detection of prostate cancer harboring adverse pathological features of intraductal carcinoma and invasive cribriform carcinoma. J Urol 2018; 200: 104– 13