Posts
Residents’ podcast: MIMIC Study
Part of the BURST/BJUI Podcast Series
Mr Chuanyu Gao is a Core Surgical Trainee in KSS Deanery. He graduated from UCL Medical School and obtained his iBSc in Surgical Sciences before completing his Academic Foundation Years in East of England Foundation School. Chuanyu first became involved with BURST on the MIMIC Study as an international site coordinator and has been part of the BURST committee ever since.
Factors associated with spontaneous stone passage in a contemporary cohort of patients presenting with acute ureteric colic: results from the Multi‐centre cohort study evaluating the role of Inflammatory Markers In patients presenting with acute ureteric Colic (MIMIC) study
Long live the BJUI
How time flies! It seems like only yesterday that I was appointed the 10th Editor‐in‐Chief of a 90‐year old major surgical journal. We assembled a dynamic team with a clear, modern vision and strategy. As we say goodbye, it is time to reflect fondly on our achievements.
The most read surgical journal on the web?
Of the many ways to measure this, one is the number of downloads of BJUI articles from our publisher Wiley Online Library. This has increased steadily every year, reaching 3 million downloads in 2019 alone. In addition to this we are regarded as pioneers of web‐based publishing and social media. The BJUI itself and its editorial team have a large, devoted following especially on Twitter. Our infographics, podcasts, picture quizzes, polls and videos were deliberately designed to grab an audience with limited time and short attention spans. The BJUI blogs have often been read more than the articles themselves, bringing immediacy, wider engagement and sensible debate. The most visited blog on the death of Nobel Laureate Tagore from prostatic enlargement was read nearly 110 000 times.
To increase the impact of the BJUI
Our impact factor has steadily increased since 2012, reaching the highest in its history and is as close to 5 as it ever has been. This has been achieved by decreasing the acceptance rate to 10% without any form of manipulation. This means that the BJUI papers are now “returnable” to any research excellence exercise of which many exist worldwide. As a clinician–scientist I could not accept anything else in academic circles. The BJUI is the only surgical journal to be rated in the Altmetric top 50 reaching a score of 1469 [1], compared to an average Altmetric score of 3. It is a testament to the hard work of our team above and beyond the impact factor. I suspect that with more fully open access journals such as the BJUI Compass , driven by Plan S, the importance of the impact factor as it now stands, may gradually diminish over time. We have also led on bringing innovation such as Artificial Intelligence [2] into our journal and making science accessible to a clinical audience through our “science made simple” section.
Quality without boundaries
While many of our papers come from the UK, USA and Australia, we have also published the best articles from Uganda, China, Japan, Iran, Korea, India, Pakistan and Peru. We are and remain a global journal, associated with 10 international societies. The NICE guidelines have been well cited over the last 3 years [3] as have the papers in our Trials section and the ever‐popular Guideline of Guidelines [4]. We have managed to co‐publish a number of high‐quality Cochrane reviews including the only one with a maximum AMSTAR score of 11 out of 11 comparing laparoscopic, robotic and open radical prostatectomy [5].
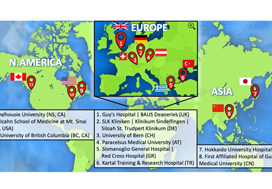
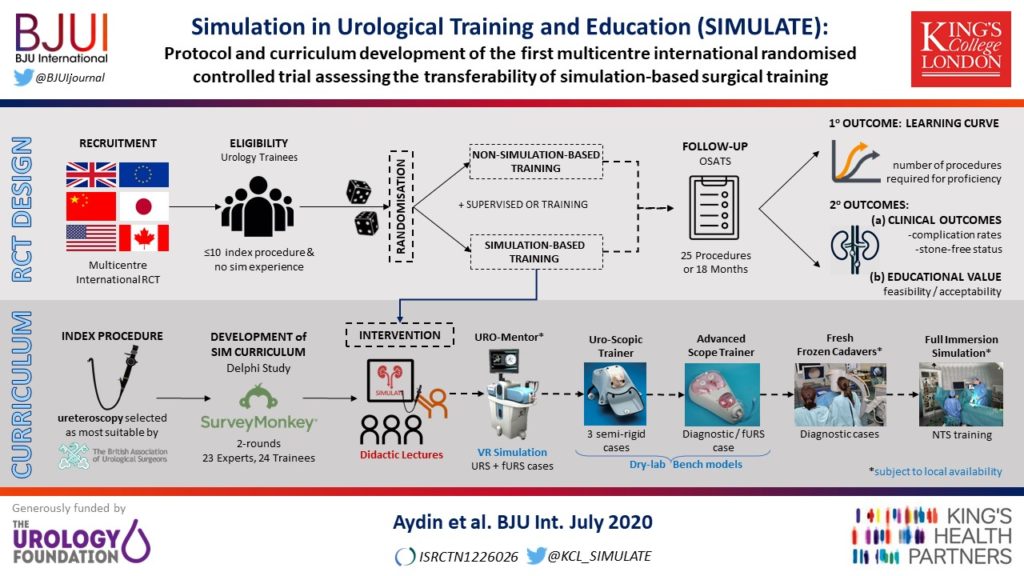
In this issue of the BJUI , we have published the protocol and curriculum development of the SIMULATE study – the world’s first and only multi‐centre randomised controlled trial of surgical simulation. What started as a BAUS study, expanded worldwide and recruited 1400 cases to see if simulation made better surgeons and improved patient outcomes [6].
The BJUI also brought innovative design from the fashion industry into academic publishing through the Glass magazine. As a parting gift, I therefore thought it fitting to publish a photograph of the courtyard of King’s College London where the SIMULATE trial first started. It was taken on a sunny day on my iPhone with no one in sight because of the pandemic. We have seen the viral crisis as an opportunity to learn from other nations and published a critical review to guide urological care for our colleagues, residents and patients [7].
I take this opportunity to thank a loyal group of friends at the BJUI Editorial offices, our trustees, the Associate and Consulting Editors, our wider editorial team of authors and reviewers and our publisher Wiley. I am proud to hand over the BJUI to my friend Freddie Hamdy in the best state of academic health and creativity.

References
- Veale D, Miles S, Bramley S et al. Am I normal? A systematic review and construction of nomograms for flaccid/erect penis length and circumference. BJU Int 2015; 115: 978– 86
- Chen J, Remulla D, Nguyen JH et al. Current status of artificial intelligence applications in urology and their potential to influence clinical practice. BJU Int 2019; 124: 567– 77
- Guidance NICE. – Prostate cancer: diagnosis and management. BJU Int 2019; 124: 9– 26
- Sussman RD, Syan R, Brucker B. Guideline of guidelines: urinary incontinence in women. BJU Int 2020; 125: 638– 55
- Ilic D, Evans SM, Allan CA et al. Laparoscopic and robot‐assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int 2018; 121: 845– 53
- Aydin A, Ahmed K, Van Hemelrijck M et al. Simulation in Urological Training and Education (SIMULATE): Protocol and curriculum development of the first multicentre international randomized controlled trial assessing the transferability of simulation‐based surgical training. BJU Int 2020; 126: 202–11
- Puliatti S, Eissa A, Eissa R et al. COVID‐19 and urology: a comprehensive review of the literature. BJU Int 2020; 125: E7– E14
BJUI journal prizes
Every year the BJUI awards three prizes to trainee urologists who have played a significant role in contributing to the work published in the journal. The prizes go towards travel costs enabling the trainees to visit international conferences. In 2020, due to the coronavirus pandemic leading to the cancellation of many of these conferences, the usual prize-giving ceremonies have not taken place so here we are introducing you to the prize winners and their work. We hope they will be able to spend their prize money in 2021.
Global prize
This is awarded to authors who are trainees based anywhere in the world other than the Americas and Europe. Usually presented at the USANZ annual meeting. In 2020 the prize was awarded to Sho Uehara for his work on artificial intelligence in prostate cancer diagnosis.
Assistant professor, Department of Urology
Tokyo Medical and Dental University
Email: [email protected]
Sho Uehara received a Ph.D. from the graduate school of Tokyo Medical and Dental University, Tokyo, Japan, in 2018. He is now working as a urologist and an assistant professor at the university hospital. His research interests include prostate cancer diagnostics, and utilization of machine learning for them.
Membership of academic societies:
JUA (The Japanese Urological Association), EAU (European Association of Urology) and AUA (American Urological Association)
Coffey-Krane prize
The Coffey-Krane prize is awarded to an author who is a trainee based in The Americas. Normally presented at the AUA annual conference. Dr Nathan Wong received this year’s award for his work on using machine learning to predict biochemical cancer recurrence following prostatectomy.
Associate Professor
Westchester Medical Center and New York Medical College
Dr Nathan Wong is an assistant professor and associate program director in the Department of Urology at Westchester Medical Center and New York Medical College. He specializes in urologic oncology and robotics surgery. His main interests are in technology, clinical trials and surgical education. He completed a Society of Urologic Oncology fellowship at Memorial Sloan Kettering Cancer Center in New York City and urology residency at McMaster University in Hamilton, Ontario in Canada.
John Blandy prize
This prize is for authors who are trainees based in Europe. Presented at the BAUS annual conference; the winner gives a presentation. This year the prize went to Nicholas Raison for his work on a RCT on cognitive training in robotic surgery.

Nicholas Raison is Vattikuti fellow at the MRC Centre for Transplantation and Mucosal Cell Biology, King’s College London and a Urology Specialist Registrar in the London Deanery.
Article of the week: Single-port robot assisted radical prostatectomy (SP-RARP): a systematic review and pooled analysis of the preliminary experiences
This is the final Article of the Week selected by the outgoing Editor-in-Chief from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
If you only have time to read one article this week, we recommend this one.
Single‐port robot‐assisted radical prostatectomy: a systematic review and pooled analysis of the preliminary experiences
Enrico Checcucci*, Sabrina De Cillis*, Angela Pecoraro*, Dario Peretti*, Gabriele Volpi*, Daniele Amparore*, Federico Piramide*, Alberto Piana*, Matteo Manfredi*, Cristian Fiori*, Riccardo Autorino†, Prokar Dasgupta‡, Francesco Porpiglia* and on behalf of the Uro-technology and SoMe Working Group of the Young Academic Urologists Working Party of the European Association of Urology
*Department of Urology, San Luigi Gonzaga Hospital, University of Turin, Turin, Italy, †Division of Urology, VCU Health, Richmond, VA, USA, and ‡King’s College London, Guy’s Hospital, London, UK
Abstract
Objective
To summarize the clinical experiences with single‐port (SP) robot‐assisted radical prostatectomy (RARP) reported in the literature and to describe the peri‐operative and short‐term outcomes of this procedure.
Material and Methods
A systematic review of the literature was performed in December 2019 using Medline (via PubMed), Embase (via Ovid), Cochrane databases, Scopus and Web of Science (PROSPERO registry number 164129). All studies that reported intra‐ and peri‐operative data on SP‐RARP were included. Cadaveric series and perineal or partial prostatectomy series were excluded.
Results
The pooled mean operating time, estimated blood loss, length of hospital stay and catheterization time were 190.55 min, 198.4 mL, 1.86 days and 8.21 days, respectively. The pooled mean number of lymph nodes removed was 8.33, and the pooled rate of positive surgical margins was 33%. The pooled minor complication rate was 15%. Only one urinary leakage and one major complication (transient ischaemic attack) were recorded. Regarding functional outcomes, pooled continence and potency rates at 12 weeks were 55% and 42%, respectively.
Conclusions
The present analysis confirms that SP‐RARP is safe and feasible. This novel robotic platform resulted in similar intra‐operative and peri‐operative outcomes to those obtained with the standard multiport da Vinci system. The advantages of single incision can be translated into a preservation of the patient’s body image and self‐esteem and cosmesis, which have a great impact on a patient’s quality of life.
Article of the week: Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for BPH
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also an editorial written by a prominent member of the urological community. Please use the comment buttons if you would like to join the conversation.
If you only have time to read one article this week, we recommend this one.
Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for benign prostatic hyperplasia: outcomes and complications of 10 years of routine clinical practice
Javier Romero-Otero*†‡, Borja García-Gómez*†, Lucía García-González*‡, Esther García-Rojo*, Pablo Abad-López*, Juan Justo-Quintas†, José Duarte-Ojeda*‡ and Alfredo Rodríguez-Antolín*
*Urology Department, Grupo de Investigación Salud Integral del Varón imas12, Hospital Universitario 12 Octubre, †Hospital Universitario HM Montepríncipe, and ‡Hospital Universitario La Luz, Madrid, Spain
Abstract
Objective
To assess the perioperative outcomes of holmium laser enucleation of the prostate (HoLEP) in real‐life practice and investigate the factors influencing the safety and effectiveness of the technique.
Patients and Methods
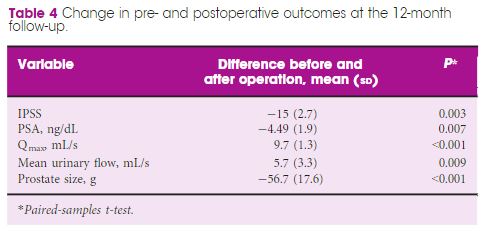
Critical analysis of patients with benign prostate hyperplasia (BPH) treated with HoLEP over 10 years of routine practice in three hospitals. Analysed variables included: preoperative characteristics (prostate size, active antiplatelet/anticoagulant therapy, blood parameters. prostate‐specific antigen (PSA) level, maximum urinary flow rate [Qmax], and International Prostate Symptom Score [IPSS]), intraoperative variables (operation time, concomitant removal of bladder calculi, and complications), early postoperative outcomes (change in blood parameters, catheterisation time, and hospital stay), and 12‐month follow‐up outcomes (change in IPSS, PSA level, and Qmax).
Results
The analysis included 963 patients, aged 48–91 years, with a mean (range) prostate size of 91 (35–247) mL. The mean (sd ) operation time was 77 (29) min, and the hospital stay and catheterisation time were 4 (2) and 1.3 (2) days, respectively. In all, 56 patients (5.6%) required concomitant removal of bladder calculi and 36 (3.7%) were converted to open prostatectomy or transurethral resection of the prostate due to intraoperative complications. Patients had a significant decrease in haemoglobin and haematocrit, but no differences were seen between patients with and without anticoagulant/antiplatelet therapy and those with prostates ≥ and <100 mL. The concomitant removal of bladder calculi and having a prostate ≥100 mL resulted in a longer operation time, but did not influence the safety and effectiveness outcomes.
Conclusions
HoLEP is suitable for real‐life patients with BPH, irrespective of the presence of active treatment with anticoagulant/antiplatelet, bladder lithiasis or a prostate ≥100 mL.
Editorial: HoLEP is the complete technique for treating BPH
Ten years of experience with holmium laser enucleation of the prostate (HoLEP) are documented by Romero‐Otero et al. [1] and offer valuable insight into the real‐world use of this technique. No information on the 10‐year durability is available, however, as only the 12‐month data are presented, but there is a wealth of other information concerning both peri‐operative outcomes and complications. A particular strength of this paper is that all‐comers were studied, including patients with catheters, those with prostates larger than 100 g and those taking anti‐coagulants, plus there is the addition of the cases the three surgeons performed during their ‘learning curve’, although these are not analysed separately.
The authors’ technique almost certainly evolved over the study period. Personally, I currently find a one‐ or two‐piece enucleation to be more efficient than the three‐lobe technique originally described [2]. Enucleation efficiency of 1–2 g/min, as was achieved in this series (73 g in 40 min), is a good benchmark for tissue removal for those new to the technique and is a good measure of surgical proficiency. Being less aggressive anteriorly seems to have an impact on continence. It is often tempting to completely enucleate circumferentially in one continuous plane which is sometimes well beyond the commissure anteriorly. A more moderate dissection in this area can reduce the transient incontinence sometimes seen [3]. The incontinence rates in the current series of 12.8% at 3 months and 2.3% at 12 months are probably representative [1]. An analysis of the factors predisposing to moderate‐to‐severe incontinence in the six patients in this series would have been useful, particularly regarding prostate size, presence of a catheter and age.
The main contribution of HoLEP to the urological armamentarium is its ability to safely treat large prostates endoscopically [4]. Although robot‐assisted techniques have also decreased the morbidity of open prostatectomy [5], the attraction of the obvious ‘natural orifice’ for access and the use of laser technology for the enucleation with HoLEP is probably the least morbid and most cost‐effective way to treat these patients. Tackling a prostate larger than 100 g involves applying the same principles as for smaller prostates, with a few provisos. Firstly, having a consistent strategy for these large prostates is important and can be reassuring when things become difficult. Secondly, it is even more important to maintain the correct plane religiously as it is easier to get lost in these glands. A good sense of direction is important! Thirdly, stay ahead of the bleeding rather than trying to catch up as it can further compound an already difficult situation. Patience is a virtue.
The learning curve of HoLEP has historically been regarded as a major barrier to the uptake of the technique [6]. This has, of course, been exaggerated by proponents of other techniques, but it is important to emphasize that during this learning phase the excellent outcomes are maintained and that conversion to TURP, if necessary (3.4% in this series), can be safely done, as these authors’ have demonstrated. The length of the learning curve has been variously described as being between 20 and 80 cases and is almost entirely due to the way training is done. A modular mentored approach appears to be the best method and could equally be applied to endoscopic enucleation using any of the other energy sources that have been described [7].
HoLEP and all its progeny are here to stay, but which of these enucleation energy sources will gain ascendancy remains to be seen. Sadly, this will likely be more to do with the depth of the corporate pockets and their commitment to the cause rather than proper scientific appraisal [8].
by Peter Gilling
References
- Romero‐Otero J, Garcia‐Gomez B, Garcia‐Gonzalez L et al. Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for benign prostatic hyperplasia: outcomes and complications of 10 years of routine clinical practice. BJU Int 2020; 126: 177-182
- Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol 1998; 12: 457– 9
- Tunc L, Yalcin S, Kaya E et al. The “Omega Sign”: a novel HoLEP technique that improves continence outcomes after enucleation. World J Urol 2020 https://doi.org/10.1007/s00345-020-03152-9
- Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser enucleation of the prostate for glands larger than 100 g: an endourologic alternative to open prostatectomy. J Endourol 2000; 14: 529– 31
- Mourmouris P, Keskin SM, Skolarikos A et al. A prospective comparative analysis of robot‐assisted vs open simple prostatectomy for benign prostatic hyperplasia. BJU Int 2019; 123: 313– 7
- Placer J, Gelabert‐Mas A, Vallmanya F et al. Holmium laser enucleation of prostate: outcome and complications of self‐taught learning curve. Urology 2009; 73: 1042– 8
- Kuronen‐Stewart C, Ahmed K, Aydin A et al. Holmium Laser Enucleation of the prostate: simulation based training curriculum and validation. Urology 2015; 86: 639– 46.
- Herrmann TR. Enucleation is enucleation is enucleation is enucleation. World J Urol 2016; 34: 1353– 5
Article of the month: SIMULATE: Protocol and curriculum development of the first multicentre international randomized controlled trial assessing the transferability of simulation‐based surgical training
Every month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also a visual abstract created by a member of the team.
If you only have time to read one article this month, we recommend this one.
Simulation in Urological Training and Education (SIMULATE): Protocol and curriculum development of the first multicentre international randomized controlled trial assessing the transferability of simulation‐based surgical training
Abdullatif Aydin*, Kamran Ahmed*†, Mieke Van Hemelrijck‡, Hashim U. Ahmed§–, Muhammad Shamim Khan* ** and Prokar Dasgupta* ** on behalf of the SIMULATE Trial Group**
*MRC Centre for Transplantation, King’s College London, London, †Department of Urology, King’s College Hospital NHS Foundation Trust, London, ‡School of Cancer and Pharmaceutical Studies, King’s College London, London, §Department of Surgery and Cancer, Imperial College London, ¶Department of Urology, Imperial College Healthcare NHS Trust, London, and **Department of Urology, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
Abstract
Objectives
To report the study protocol for the first international multicentre randomized controlled trial investigating the effectiveness of simulation‐based surgical training and the development process for an evidence‐based training curriculum, to be delivered as an educational intervention.
Participants and Methods
This prospective, international, multicentre randomized controlled clinical and educational trial will recruit urology surgical trainees who must not have performed ≥10 of the selected index procedure, ureterorenoscopy (URS). Participants will be randomized to simulation‐based training (SBT) or non‐simulation‐based training (NSBT), the latter of which is the current sole standard of training globally. The primary outcome is the number of procedures required to achieve proficiency, where proficiency is defined as achieving a learning curve plateau of 28 or more on an Objective Structured Assessment of Technical Skills (OSATS) assessment scale, for three consecutive operations, without any complications. All participants will be followed up either until they complete 25 procedures or for 18 months. Development of the URS SBT curriculum took place through a two‐round Delphi process.
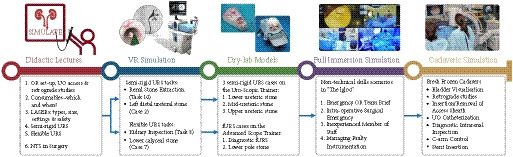
Results
A total of 47 respondents, consisting of trainees (n = 24) with URS experience and urolithiasis specialists (n = 23), participated in round 1 of the Delphi process. Specialists (n = 10) finalized the content of the curriculum in round 2. The developed interventional curriculum consists of initial theoretic knowledge through didactic lectures followed by select tasks and cases on the URO‐Mentor (Simbionix, Lod, Israel) VR Simulator, Uro‐Scopic Trainer (Limbs & Things, Bristol, UK) and Scope Trainer (Mediskills, Manchester, UK) models for both semi‐rigid and flexible URS. Respondents also selected relevant non‐technical skills scenarios and cadaveric simulation tasks as additional components, with delivery subject to local availability.
Conclusions
SIMULATE is the first multicentre trial investigating the effect and transferability of supplementary SBT on operating performance and patient outcomes. An evidence‐based training curriculum is presented, developed with expert and trainee input. Participants will be followed and the primary outcome, number of procedures required to proficiency, will be reported alongside key clinical secondary outcomes, (ISCRTN 12260261).
Article of the week: Management of large renal stones with super‐mini percutaneous nephrolithotomy: an international multicentre comparative study
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also a visual abstract created by Cora Griffin from King’s College London.
If you only have time to read one article this week, we recommend this one.
Management of large renal stones with super-mini percutaneous nephrolithotomy: an international multicentre comparative study
Yang Liu*, Chao Cai*, Albert Aquino†, Shabir Al-Mousawi‡, Xuepei Zhang§, Simon K.S. Choong¶, Xiang He**, Xianming Fan††, Bin Chen‡‡, Jianhua Feng§§, Xuhui Zhu¶¶, Abdulla Al-Naimi***, Houping Mao†††, Huilong Tang‡‡‡, Dayong Jin§§§, Xiancheng Li¶¶¶, Fenghong Cao****, Hua Jiang††††, Yongfu Long‡‡‡‡, Wei Zhang§§§§, Gang Wang¶¶¶¶, Zihao Xu*, Xin Zhang*, Shanfeng Yin* and Guohua Zeng*
*Department of Urology, Guangdong Key Laboratory of Urology, Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, †Department of Urology, Jose R. Reyes Memorial Medical Center, Manila, Philippines, ‡Division of Urology, SABAH ALAHMAD Urology Center, Ministry of Health, Al-Amiri Hospital, Kuwait City, Kuwait, §Department of Urology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, ¶Institute of Urology, University College London Hospitals, London, UK, **Department of Urology, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, ††Department of Urology, The Third Affiliated Hospital of Xiamen, The Third Affiliated Hospital of Fujian University of Traditional Chinese Medicine, ‡‡Department of Urology, The Affiliated Hospital of Xiamen University, Xiamen, §§Department of Urology, Longgang District Central Hospital, Shenzhen, ¶¶Department of Urology, Beijing Chaoyang Hospital, Affiliated to Capital Medical University, Beijing, China, ***Department of Urology, Hamad Medical Corporation, Doha, Qatar, †††Department of Urology, First Affiliated Hospital of Fujian Medical University, Fuzhou, ‡‡‡Department of Urology, The First Hospital of Hunan University of Traditional Chinese Medicine, Changsha, §§§Department of Urology, Liaoyuan City Central Hospital, Liaoyuan, ¶¶¶Department of Urology, Second Affiliated Hospital of Dalian Medical University, Dalian, ****Department of Urology, North China University of Science and Technology Affiliated Hospital, Tangshan, ††††Department of Urology, Zhongda Hospital Southeast Hospital, Nanjing, ‡‡‡‡Department of Urology, Central Hospital of Shaoyang, Shaoyang, §§§§Department of Urology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, and ¶¶¶¶Department of Urology, National Urological Cancer Center, Institute of Urology, Peking University First Hospital, Peking University, Beijing, China
Abstract
Objectives
To comparatively evaluate the clinical outcomes of super‐mini percutaneous nephrolithotomy (SMP) and mini‐percutaneous nephrolithotomy (Miniperc) for treating urinary tract calculi of >2 cm.
Patients and Methods
An international multicentre, retrospective cohort study was conducted at 20 tertiary care hospitals across five countries (China, the Philippines, Qatar, UK, and Kuwait) between April 2016 and May 2019. SMP and Miniperc were performed in 3525 patients with renal calculi with diameters of >2 cm. The primary endpoint was the stone‐free rate (SFR). The secondary outcomes included: blood loss, operating time, postoperative pain scores, auxiliary procedures, complications, tubeless rate, and hospital stay. Propensity score matching analysis was used to balance the selection bias between the two groups.
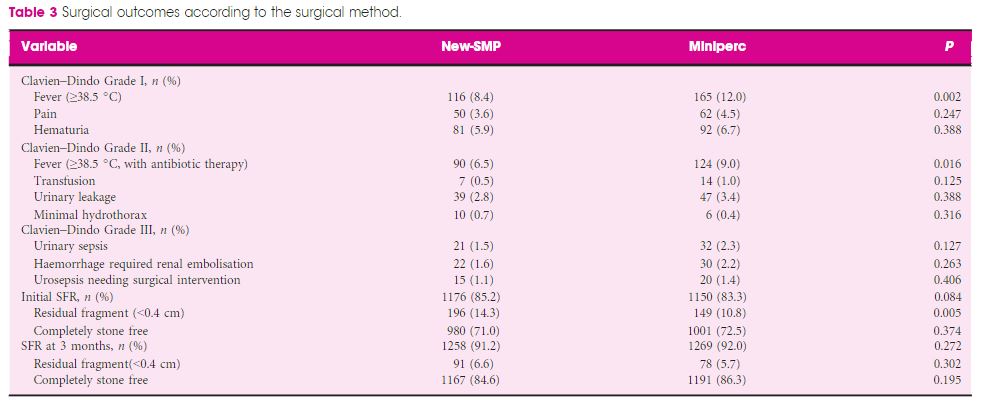
Results
In all, 2012 and 1513 patients underwent SMP and Miniperc, respectively. After matching, 1380 patients from each group were included for further analysis. Overall, there was no significant difference in the mean operating time or SFR between the two groups. However, the hospital stay and postoperative pain score were significantly in favour of SMP (both P < 0.001). The tubeless rate was significantly higher in the SMP group (72.6% vs 57.8%, P < 0.001). Postoperative fever was much more common in the Miniperc group (12.0% vs 8.4%, P = 0.002). When the patients were further classified into three subgroups based on stones diameters (2–3, 3–4, and >4 cm). The advantages of SMP were most obvious in the 2–3 cm stone group and diminished as the size of the stone increased, with longer operating time in the latter two subgroups. Compared with Miniperc, the SFR of SMP was comparable for 3–4 cm stones, but lower for >4 cm stones. There was no statistical difference in blood transfusions and renal embolisations between the two groups.
Conclusions
Our data showed that SMP is an ideal treatment option for stones of <4 cm and is more efficacious for stones of 2–3 cm, with lesser postoperative fever, blood loss, and pain compared to Miniperc. SMP was less effective for stones of >4 cm, with a prolonged operating time.