Paediatric urology in the BJUI
 The BJUI and the Editorial team are committed to the publication of high-quality and highly citable articles concerning translational science for the International Paediatric Urology Community. We encourage authors to submit original and outstanding work for publication that can influence clinical practice or introduce innovative new care methods for children across the world.
The BJUI and the Editorial team are committed to the publication of high-quality and highly citable articles concerning translational science for the International Paediatric Urology Community. We encourage authors to submit original and outstanding work for publication that can influence clinical practice or introduce innovative new care methods for children across the world.On this note we have included the best three articles in the ‘Paediatrics’ section in this month’s issue.
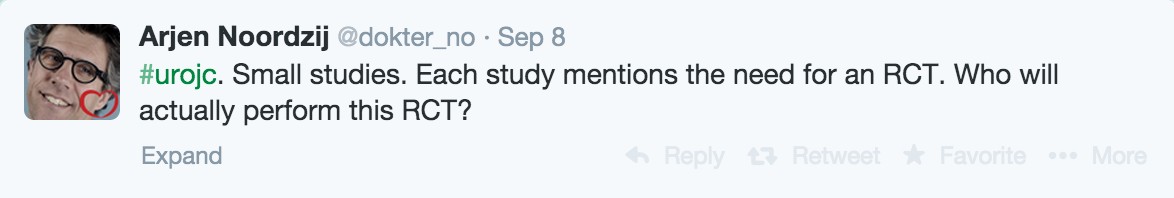
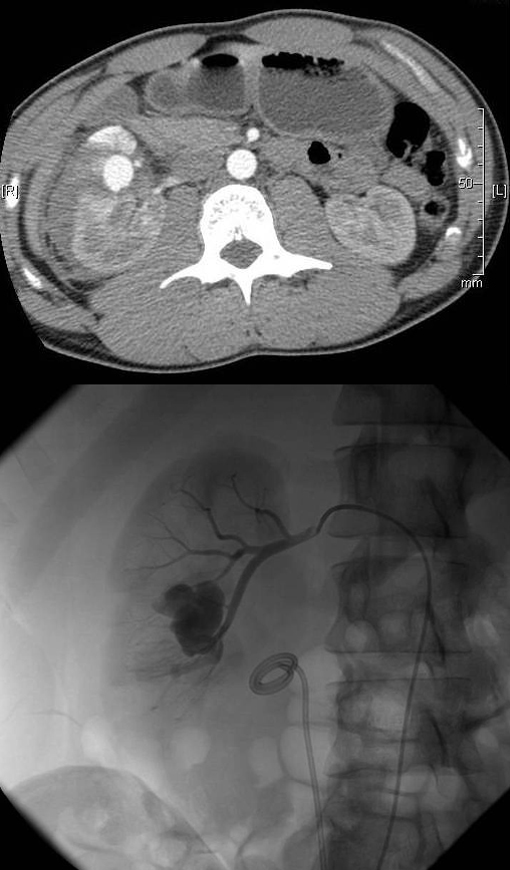
Cundy et al. [1] from London (UK), have to be commended for the thoughtful meta-analysis of robot-assisted pyeloplasty (RAP).This is an early, but, timely analysis of our current practice of different approaches to paediatric pyeloplasty. The primary outcomes were not significantly different for the open, robotic or laparoscopic approaches. This is not surprising ,as the surgeons that used these new approaches have been proficient with their traditional approaches and have embraced the newer techniques with caution. RAP had a distinct advantage of reduced analgesia and length of hospital stay compared with the traditional open approaches, and this will probably drive the adoption of the newer approaches even at the expense of increased cost. Hopefully, the cost issue will be transient; as the new technology becomes increasingly widespread the cost should level out. Randomised clinical trials may be an answer to newer treatment adoption,but this may not be possible in all scenarios – hence a prospective comparative series may answer the question, with some human factor bias [2]. The advantage of ergonomic comfort and a reduced learning curve for surgeons performing these reconstructive procedures using the robotic approach,as mentioned by the authors,has the benefit of reducing professional health hazards and saving on human capital. Unfortunately, this has never been considered or measured, although it is an important aspect.
Suer et al. [3] from Turkey, have analysed their anti-reflux surgery series in children using the open approach to predict complications in a multivariate analysis. The utmost factor is bladder dysfunction, e.g.bladder-bowel dysfunction, dysfunctional elimination syndrome or dysfunctional voiding. Over the years paediatric urologists have found this to be associated with VUR and poor outcomes after surgery. Extreme caution has to be taken when deciding to perform surgery in this group, as theVUR may be secondary and surgery may not be warranted at all.Ureteric tapering or tailoring of the dilated ureter is another factor for poor outcomes, which can be attributed to the poor vascularity of chronically dilated ureters. This practice has been based on the physics of Paquin’s law.Unfortunately, we do not have evidence of outcomes without this reduction plasty on these ureters. The authors have also emphasised the limitations of the current adult Clavien system of classification used for grading [4], which has pitfalls and does not describe the complications well either in the paediatric population. It is an appeal to the paediatric urology community for further work to be done to produce a standardised grading system for use in paediatric cases.
Dangle et al. [5] from The University of Chicago have attempted to describe extravesical robotic ureteric re-implantation for VUR in children. The technique of re-implantation has not been described well to date, although there have been a few outcome reports with variable success rates. This explains the fact there may not be uniformity in this technique and/or the learning curve. The surgery itself is challenging because of the close proximity of important anatomical structures within a confined space, and the risk of ureteric damage with improper handling is unforgiving. The video describes their current modified technique with important surgical steps for adoption. The success rate for resolution is still, not on a par with open surgery, but there were no complications. The fine balance between success and complications needs to be defined for incorporation into the paediatric urological armamentarium.
Moving forward:
‘With availability of advanced automated instruments to replace manual labour, if as a society we prefer this at an increased cost, then why not on the same philosophy adopt these new technologies in the surgical realm with proper training and safety to reduce the morbidity and achieve at par results?’.
and
‘The surgical dogma of practice needs to be challenged with evidence-based outcomes to move ahead’.
Conflict of Interest
None declared.
Mohan S. Gundeti, MD, MCh, FEBU, FRCS, FEAPU
BJUI Consulting Editor–Paediatrics, The University of Chicago Medicine, Chicago, IL, USA e-mail: [email protected]
References
1 Cundy TP, Harling L, Hughes-Hallett A et al. Meta-analysis of robot-assisted vs conventional laparoscopic and open pyeloplasty in children. BJU Int 2014; 114: 582–94
2 Orvieto MA, Large M, Gundeti MS. Robotic paediatric urology.BJU Int 2012; 110: 2–13
3 Suer E, Ozcan C, Mermerkaya M et al. Can factors affecting complication rates for ureteric re-implantation be predicted? Use of the modified Clavien classification system in a paediatric population. BJU Int 2014; 114: 595–600
4 Clavien PA, Barkun J, de Oliveira ML et al. The Clavien-Dindo classification of surgical complications: five-year experience.Ann Surg 2009; 250: 187–96
5 Dangle PP, Shah A, Gundeti MS. Robot-assisted laparoscopic ureteric reimplantation:extravesical technique. BJU Int 2014; 114: 630–2
© 2014 The Author 468 BJU International © 2014 BJU International