Editorial: How many cores are needed to detect nearly all prostate cancers?
Virtual prostate biopsy and biopsy simulation: lessons to be learned
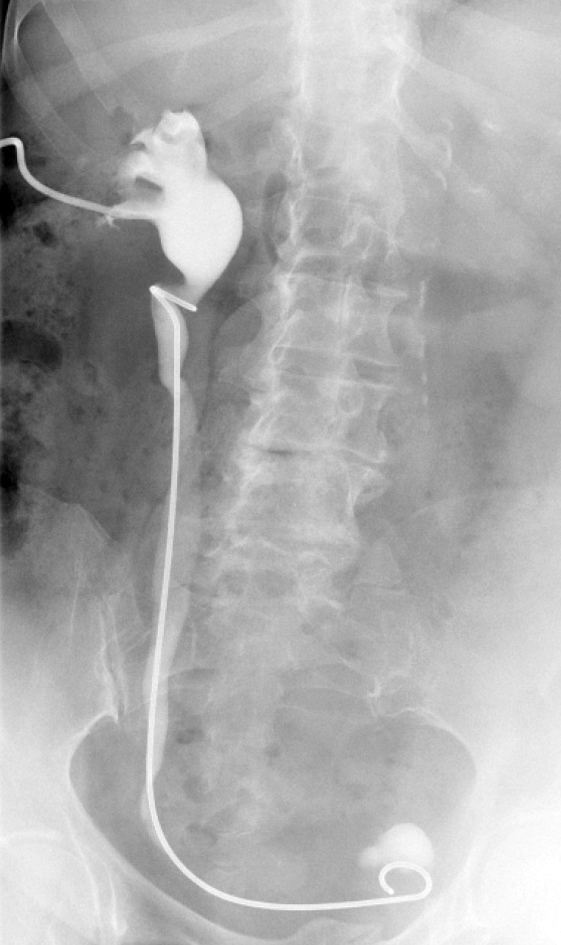
Prostate biopsies, transrectal or transperineal, still constitute the pillars of prostate cancer detection today [1]. With the lack of reliable imaging tools (new MRI techniques are promising but still investigational [2]); random biopsies offer the sole adequate cancer detection option [3]. However, random biopsies are far from efficient in detecting all tumours and even less efficient in detecting all significant cancer ‘spots’. To improve sensitivities and specificities, increasing the biopsy core numbers, targeting more lateral aspects and encouraging repeat biopsies have been recommended [4]. Recently, HistoScanning™ [5] and template biopsies [6] have been introduced to further improve biopsy quality and efficiency. The latest innovations include the fusion of MRI pictures with the TRUS image to offer optimal targeting of suspicious areas [7]. And yet, these efforts are far from solving the main problem. How can we perform a biopsy and be confident to detect most of the cancers, i.e. significant malignant areas.
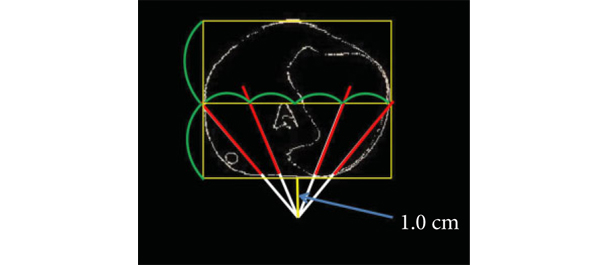
The present study [1] does, what should have been done a long time ago, namely to create a reliable and reproducible biopsy simulation model to allow the investigation of various biopsy schemes, core lengths and numbers. Based on a series of 109 radical prostatectomy specimens, a three-dimensional (3D) prostate and prostate cancer model was created using novel 3D slicer software and various prostate biopsy schemes were simulated. Using this method, the detection rate for tumours with a tumour volume (TV) of ≥0.5 mL plateaued at 77% (69 of 90) using a 12 core (3 × 4) scheme, standard 17-mm biopsy cutting length without anteriorly directed biopsy (ADBx) cores. Twenty of 21 (95%) tumours with a TV of ≥0.5 mL not detected by this scheme originated in the anterior peripheral zone or transition zone [1].
Confirming our earlier data with the Vienna nomograms [8], increasing the biopsy cutting length and depth/number of ADBx cores (14–18 cores) improved the detection rate for tumours with a TV of ≥0.5 mL in the 12-core scheme [1]. The best biopsy scheme used a 22-mm cutting length and a 12-core scheme with additional volume-adjusted ADBx cores. Using this combination, 100% of ≥0.5 mL tumours in prostates <50 mL in volume and 94.7% of ≥0.5 mL tumours in prostates >50 mL in volume were detected.
Certainly, these numbers will not be reproducible in real-time TRUS or transperineal biopsies (detections rates of 95–100% as seen in this simulation model, cannot be achieved without adequate imaging tools, which are not available yet), but they aid significantly in rethinking our biopsy strategy. So, if we summarise the present findings and combine them with published data, the future will demand a TRUS-fusion biopsy technique, involving 14–18 cores (or more if volume increases), involving the anterior zones of the prostate and using a 22-mm cutting length of the biopsy core vs a 15–17 mm core as is used currently. Obviously real-time prospective trials are needed to confirm these findings but nothing indicates that the outcome would be otherwise.
Bob Djavan
Department of Urology, New York University School of Medicine, NYU, New York, NY, USA
References
- Kanao K, Eastham JA, Scardino PT, Reuter VE, Fine SW. Can transrectal needle biopsy be optimised to detect nearly all prostate cancer with a volume of ≥0.5 mL? A three-dimensional analysis. BJU Int 2013; 112: 898–904
- Delongchamps NB, Peyromaure M, Schull A et al. Pre-biopsy Magnetic Resonance Imaging and prostate cancer detection: comparison of random and MRI-targeted biopsies using three different techniques of MRI-TRUS image registration. J Urol 2013;189: 493–499
- Djavan B, Rocco B. Optimising prostate biopsy. BMJ 2011; 344: d8201
- Thompson I, Thrasher JB, Aus G et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol 2007; 177: 2106–2131
- Simmons LA, Autier P, Zát’ura F et al. Detection, localisation and characterisation of prostate cancer by prostate HistoScanning(™). BJU Int 2012; 110: 28–35
- Huo AS, Hossack T, Symons JL et al. Accuracy of primary systematic template guided transperineal biopsy of the prostate for locating prostate cancer: a comparison with radical prostatectomy specimens. J Urol 2012; 187: 2044–2049
- Sonn GA, Natarajan S, Margolis DJ et al. Targeted biopsy in the detection of prostate cancer using an office based magnetic resonance ultrasound fusion device. J Urol 2013; 189: 86–92
- Djavan B, Margreiter M. Biopsy standards for detection of prostate cancer. World J Urol 2007; 25: 11–17