Editorial: Robotic and conventional open radical cystectomy lead to similar postoperative health-related quality of life
In this month’s issue of BJU International, Messer et al. [1] devise a prospective randomised trial to compare postoperative health-related quality of life (HRQoL) after robot-assisted (RARC) vs conventional open radical cystectomy (ORC). The investigators evaluated 40 patients over a follow-up period of 1 year and found no significant difference in HRQoL between surgical approaches. Moreover, they showed that the postoperative decrease in HRQoL returns to baseline within 3 months of surgery.
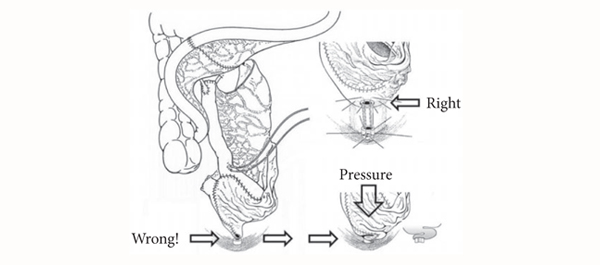
RC is one of the most challenging and potentially mutilating surgical interventions in the urological field and represents the standard-of-care treatment for patients with muscle-invasive bladder cancer. It is associated with a non-negligible risk of morbidity and mortality [2]. With the advent of new technologies, such as the Da Vinci surgical robot, carefully designed studies are needed to weigh the potential benefits of a novel approach against the increased costs associated with such tools. While RARC holds the promise of combining the benefits of a minimally invasive intervention with the precise robotic translation of the surgeon’s movements, these claims remain to be definitely proven in the clinical setting. As such, further elucidating the effect of surgical approach on perioperative outcomes after RC is essential for treatment planning, patient counselling and informed decision-making before surgery.
QoL is increasingly used as a quantitative measure of treatment success [3, 4]. These measures are gaining considerable traction in the USA, as reimbursements will soon be tied to patient satisfaction. While previous retrospective studies suggest that RARC has comparable perioperative oncological outcomes with potentially lower morbidity relative to ORC [5], there is a scarcity of high-quality evidence on HRQoL outcomes of RARC vs ORC. The difficulties of conducting randomised trials in the surgical setting are reflected by the relatively few participants in the Messer et al. [1] trial. Nonetheless, in their pilot study, the authors demonstrated the feasibility of a HRQoL trial in RC patients. Furthermore, they deliver initial evidence on the impact of surgical approach on HRQoL after RC.
From a clinical perspective, the authors contribute interesting findings to the ongoing debate. Their results suggest that the potential benefits of robot-assisted surgery on HRQoL may be limited in patients undergoing complex oncological surgery such as RC. Several hypotheses may be pertinent to their conclusions. For example, performing an open urinary diversion after RARC that can take as much time as the actual extirpative RC may mitigate any potential benefit of the minimally invasive approach. Furthermore, the study findings may be largely influenced by the surgical skills of the participating surgeons. Maybe the correct interpretation of their study findings is that there was no significant difference in HRQoL outcomes between ORC and RARC, at the institution where the trial was performed.
Nonetheless, the authors suitably demonstrate the feasibility of performing a randomised trial in this field and pave the way towards adequately powered, randomised multicentre trials that can provide further evidence on what impact RARC may have on perioperative outcomes and beyond.
Julian Hanske, Florian Roghmann, Joachim Noldus and Quoc-Dien Trinh*
Department of Urology, Marien Hospital, Ruhr-University Bochum, Herne, Germany, and *Division of Urologic Surgery and Center for Surgery and Public Health, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
References
1 Messer JC, Punnen S, Fitzgerald J, Svatek R, Parekh DJ. Health-related quality of life from a prospective randomised clinical trial of robot-assisted laparoscopic vs open radical cystectomy. BJU Int 2014; 114: 896–902
2 Roghmann F, Trinh QD, Braun K et al. Standardized assessment of complications in a contemporary series of European patients undergoing radical cystectomy. Int J Urol 2014; 21: 143–9
3 Cookson MS, Dutta SC, Chang SS, Clark T, Smith JA Jr, Wells N. Health related quality of life in patients treated with radical cystectomy and urinary diversion for urothelial carcinoma of the bladder: development and validation of a new disease specific questionnaire. J Urol 2003; 170: 1926–30
4 Loppenberg B, von Bodman C, Brock M, Roghmann F, Noldus J, Palisaar RJ. Effect of perioperative complications and functional outcomes on health-related quality of life after radical prostatectomy. Qual Life Res 2014. doi: 10.1007/s11136-014-0729-1
5 Kader AK, Richards KA, Krane LS, Pettus JA, Smith JJ, Hemal AK. Robot-assisted laparoscopic vs open radical cystectomy: comparison of complications and periopera