Article of the Week: HAL fluorescence cystoscopy in the diagnosis of NMIBC
Every Week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Effectiveness of hexaminolevulinate fluorescence cystoscopy for the diagnosis of non-muscle-invasive bladder cancer in daily clinical practice: a Spanish multicentre observational study
OBJECTIVE
To assess the sensitivity and specificity of blue-light cystoscopy (BLC) with hexaminolevulinate as an adjunct to white-light cystoscopy (WLC) vs WLC alone for the detection of non-muscle-invasive bladder cancer (NMIBC), in routine clinical practice in Spain.
PATIENTS AND METHODS
An intra-patient comparative, multicentre, prospective, observational study. Adults with suspected or documented primary or recurrent NMIBC at eight Spanish centres were included in the study. All patients were examined with WLC followed by BLC with hexaminolevulinate. We evaluated the detection rate of bladder cancer lesions by WLC and BLC with hexaminolevulinate, overall and by tumour stage and compared with histological examination of the biopsied lesions. Sensitivity and specificity was calculated.
RESULTS
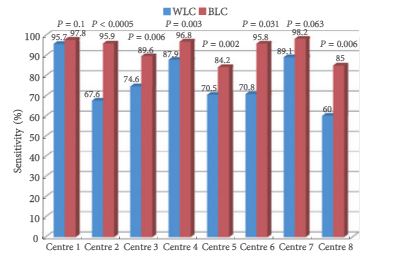
In all, 1 569 lesions were identified from 283 patients: 621 were tumour lesions according to histology and 948 were false-positives. Of the 621 tumour lesions, 475 were detected by WLC (sensitivity 76.5%, 95% confidence interval [CI] 73.2–79.8) and 579 were detected by BLC (sensitivity 93.2%, 95% CI 91.0–95.1; P < 0.001). There was a significant improvement in the sensitivity in the detection of all types of NMIBC lesions with BLC compared with WLC. Of 219 patients with tumours, 188 had NMIBC [highest grade: carcinoma in situ (CIS), n = 36; Ta, n = 87; T1, n = 65). CIS lesions were identified more with BLC (n = 27) than with WLC [n = 19; sensitivity: BLC 75.0% (95% CI 57.8–87.9) vs WLC 52.8% (95% CI 35.5–69.6); P = 0.021]. Results varied across centres.
CONCLUSIONS
This study shows that improvement in diagnosis of NMIBC, mainly CIS and Ta tumours, obtained with BLC with hexaminolevulinate as an adjunct to WLC vs WLC alone can be shown in routine clinical practice.