Article of the week: Prostate cancer in kidney transplant recipients – a nationwide register study
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to this post, there is an editorial written by a prominent member of the urological community and a video produced by the authors. Please use the comment buttons below to join the conversation.
If you only have time to read one article this week, we recommend this one.
Prostate cancer in kidney transplant recipients – a nationwide register study
Ola Bratt*†, Linda Drevin‡, Karl-Göran Prütz§, Stefan Carlsson¶, Lars Wennberg** and Pär Stattin††
*Department of Urology, Institute of Clinical Science, Sahlgrenska Academy, Gothenburg University, †Department of Urology, Sahlgrenska University Hospital, Gothenburg, ‡Regional Cancer Centre, Uppsala-Orebro, Uppsala, §Swedish Renal Registry, Ryhov Hospital, Jönköping, ¶Section of Urology, Department of Molecular Medicine and Surgery, Karolinska Institute, **Department of Transplantation Surgery, Karolinska University Hospital, Stockholm, and ††Department of Surgical Sciences, Uppsala University, Uppsala, Sweden
Abstract
Objective
To investigate whether post‐transplantation immunosuppression negatively affects prostate cancer outcomes in male kidney transplant recipients.
Patients and Methods
We used the Swedish Renal Register and the National Prostate Cancer Register to identify all kidney transplantation recipients diagnosed with prostate cancer in Sweden 1998–2016. After linking these registers with Prostate Cancer Database Sweden (PCBaSe), a case‐control study was designed to compare time period and risk category‐specific probabilities of a prostate cancer diagnosis amongst kidney transplantation recipients versus the male general population. The registers did not include information about the specific immunosuppression agent used in all transplantation recipients. Data from PCBaSe were used to compare prostate cancer characteristics at diagnosis and survival for patients with prostate cancer with versus without a kidney transplant. Propensity score matching, Cox regression analysis and Fisher’s exact test were used and 95% confidence intervals (CIs) calculated.
Results
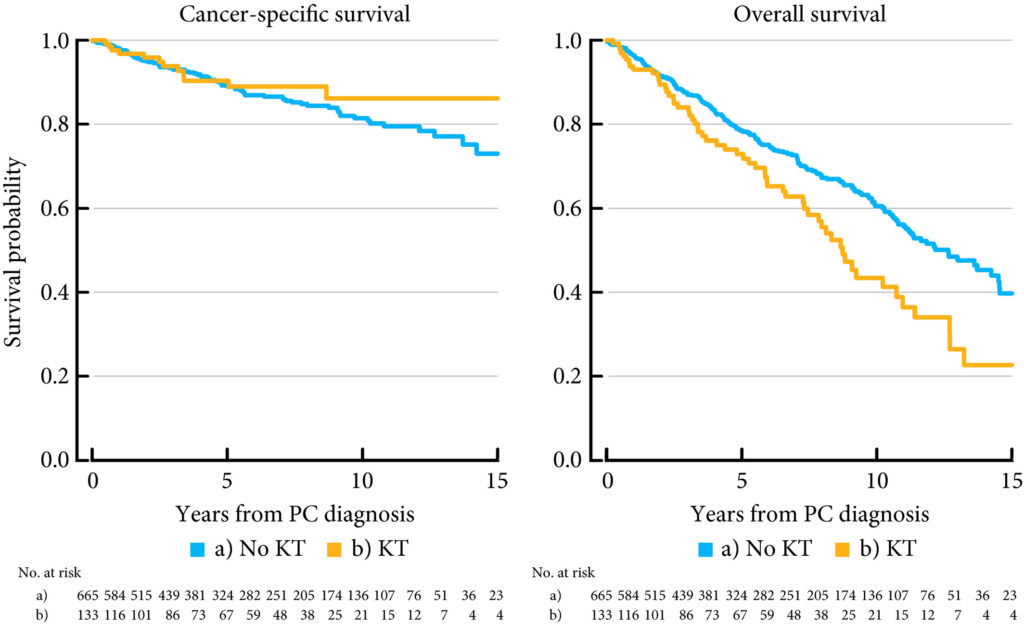
Almost half of the 133 kidney transplantation recipients were transplanted before the mid‐1990s, when PSA testing became common in cancer centers. The transplant recipients were not more likely than age‐matched control men to be diagnosed with any (odds ratio [OR] 0.84, 95% CI 0.70–0.99) or high‐risk or metastatic prostate cancer (OR 0.84, 95% CI 0.62–1.13). None of the ORs for the different categories of prostate cancer increased with time since transplantation. Cancer characteristics at the time of diagnosis and cancer‐specific survival were similar amongst transplant recipients and the control group of 665 men diagnosed with prostate cancer without a kidney transplant.
Conclusions
This Swedish nationwide, register‐based study gave no indication that immunosuppression after kidney transplantation increases the risk of prostate cancer or adversely affects prostate cancer outcomes. The study suggests that men with untreated low‐grade prostate cancer can be accepted for transplantation.



