Posts
Article of the Week: Trifecta and Optimal Peri-operative outcomes of Robotic and Laparoscopic Partial Nephrectomy In Surgical Treatment Of SRMs
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Month heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Jihad Kaouk discussing his paper.
If you only have time to read one article this week, it should be this one.
Trifecta and Optimal Peri-operative outcomes of Robotic and Laparoscopic Partial Nephrectomy In Surgical Treatment Of Small Renal Masses: A Multi-Institutional Study
OBJECTIVE
To compare the perioperative outcomes of robotic partial nephrectomy (RPN) with laparoscopic PN (LPN) performed for small renal masses (SRMs), in a large multi-institutional series and to define a new composite outcome measure, termed ‘optimal outcome’ for the RPN group.
PATIENTS AND METHODS
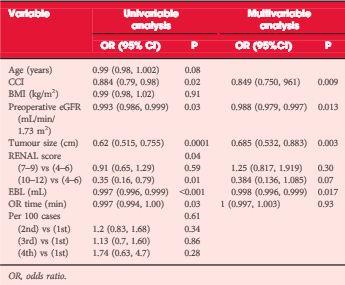
Retrospective review of 2392 consecutive cases of RPN and LPN performed in five high-volume centres from 2004 to mid-2013. We limited our study to SRMs and cases performed by surgeons with significant expertise with the technique. The Trifecta was defined as negative surgical margin, zero perioperative complications and a warm ischaemia time of ≤25 min. The ‘optimal outcome’ was defined as achievement of Trifecta with addition of 90% estimated glomerular filtration rate preservation and no chronic kidney disease stage upgrading. Univariable and multivariable analysis were used to identify factors predicting Trifecta and ‘optimal outcome’ achievement.
RESULTS
In all, 1185 RPN and 646 LPN met our inclusion criteria. Patients in the RPN group were older and had a higher median Charlson comorbidity index and higher R.E.N.A.L. nephrometry score. The RPN group had lower warm ischaemia time (18 vs 26 min), overall complication rate (16.2% vs 25.9%), and positive surgical margin rate (3.2% vs. 9.7%). There was a significantly higher Trifecta rate for RPN (70% vs 33%) and the rate of achievement of ‘optimal outcome’ for the RPN group was 38.5%.
CONCLUSIONS
In this large multi-institutional series RPN was superior to LPN for perioperative surgical outcomes measured by Trifecta. Patients in the RPN group had better outcomes for all three components of Trifecta compared with their LPN counterparts. Our more strict definition for ‘optimal outcome’ might be a better tool for assessing perioperative and functional outcomes after minimally invasive PN. This tool needs to be externally validated.
Editorial: Robotic Partial Nephrectomy: The Treatment of Choice for Minimally Invasive Nephron Sparing Surgery
Early in the adoption of robotic partial nephrectomy (RPN) as an alternative to laparoscopic PN (LPN) for the treatment of small renal masses, several of the current authors presented a similar comparison of LPN and RPN. They found RPN to result in shorter hospital stay, less blood loss, and shorter warm ischaemia time (WIT) compared with LPN [1]. They discovered that RPN outcomes were not dependent on the complexity of the tumour, which clearly impacted LPN results. They concluded that RPN is a safe and viable alternative to LPN and offered benefits even for experienced laparoscopic surgeons.
The current report in this edition of BJUI furthers the comparison of RPN and LPN and expands the assessment to include five high-volume centres of excellence in robotic surgery [2]. This retrospective, multi-institutional review of 1 185 RPN and 646 LPN represents the largest comparison to date of these two approaches for minimally invasive PN. Despite higher patient comorbidities and R.E.N.A.L. nephrometry scores in the RPN patients compared with the LPN group, there were fewer overall complications (16.2% vs 25.9%), a lower positive surgical margin rate (3.2% vs 9.7%) and a lower WIT (18 vs 26 min). They also found a much higher percentage of RPN patients (70% vs 33%) meeting the Trifecta criteria, defined as negative surgical margins, no perioperative complications, and a WIT of ≤25 min. Finally, the authors introduce a more stringent composite measure of ‘optimal outcomes’, which is the Trifecta with the addition of 90% estimated GFR preservation and no chronic kidney disease upgrading. They report 38.5% of RPN patients meeting optimal outcomes compared with 24.1% for LPN.
This study clearly demonstrates the superiority of RPN over LPN and is supported by other single-surgeon reports [3]. These results also exceed those reported for open PN with the added benefit of reduced hospital stay [4]. However, it is important to recognise that these results represent a mature experience with RPN by the leaders in the field of robotic renal surgery. Many of these authors pioneered the techniques currently used for RPN, and therefore these results may not apply to centres without the same experience or case volumes. One limitation of this report is the non-concurrent experience of LPN and RPN. The results of RPN came after an initial experience with LPN and therefore the outcomes of RPN may have benefitted from the lessons learned with LPN prior to RPN.
Reporting surgical outcomes as composite results, such as the Trifecta, allows for comparison between reports and sets an outcomes bar for future studies. Most composite measures include assessment of surgical margin status and complications, but there is no current agreement as to the optimal measure of renal functional outcomes. The current Trifecta used a WIT of ≤25 min as a measure of renal function impact, while the margin, ischaemia, and complications (MIC) score uses a WIT of <20 min [5], and others have used 90% renal parenchyma preservation as part of the Trifecta [6]. The impact of WIT on renal function has been questioned given the recently recognised importance of preserved renal parenchyma as an important predictor of renal function after PN [7]. Until there is consensus as to the best measure of renal function after nephron-sparing surgery, composite outcomes such as the Trifecta and the optimal outcomes as described by the authors will have limited utility.
Video: Trifecta and Optimal Peri-operative outcomes of Robotic and Laparoscopic Partial Nephrectomy In Surgical Treatment Of SRMs
Trifecta and Optimal Peri-operative outcomes of Robotic and Laparoscopic Partial Nephrectomy In Surgical Treatment Of Small Renal Masses: A Multi-Institutional Study
OBJECTIVE
To compare the perioperative outcomes of robotic partial nephrectomy (RPN) with laparoscopic PN (LPN) performed for small renal masses (SRMs), in a large multi-institutional series and to define a new composite outcome measure, termed ‘optimal outcome’ for the RPN group.
PATIENTS AND METHODS
Retrospective review of 2392 consecutive cases of RPN and LPN performed in five high-volume centres from 2004 to mid-2013. We limited our study to SRMs and cases performed by surgeons with significant expertise with the technique. The Trifecta was defined as negative surgical margin, zero perioperative complications and a warm ischaemia time of ≤25 min. The ‘optimal outcome’ was defined as achievement of Trifecta with addition of 90% estimated glomerular filtration rate preservation and no chronic kidney disease stage upgrading. Univariable and multivariable analysis were used to identify factors predicting Trifecta and ‘optimal outcome’ achievement.
RESULTS
In all, 1185 RPN and 646 LPN met our inclusion criteria. Patients in the RPN group were older and had a higher median Charlson comorbidity index and higher R.E.N.A.L. nephrometry score. The RPN group had lower warm ischaemia time (18 vs 26 min), overall complication rate (16.2% vs 25.9%), and positive surgical margin rate (3.2% vs. 9.7%). There was a significantly higher Trifecta rate for RPN (70% vs 33%) and the rate of achievement of ‘optimal outcome’ for the RPN group was 38.5%.
CONCLUSIONS
In this large multi-institutional series RPN was superior to LPN for perioperative surgical outcomes measured by Trifecta. Patients in the RPN group had better outcomes for all three components of Trifecta compared with their LPN counterparts. Our more strict definition for ‘optimal outcome’ might be a better tool for assessing perioperative and functional outcomes after minimally invasive PN. This tool needs to be externally validated.
Article of the week: Remote ischaemic preconditioning reduces injury during partial nephrectomy
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video by Dr. Huang and colleagues to accompany their article.
If you only have time to read one article this week, it should be this one.
Effect of remote ischaemic preconditioning on renal protection in patients undergoing laparoscopic partial nephrectomy: a ‘blinded’ randomised controlled trial
Jiwei Huang, YongHui Chen, Baijun Dong, Wen Kong, Jin Zhang, Wei Xue, DongMing Liu and Yiran Huang
Department of Urology, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
OBJECTIVE
• To evaluate whether remote ischaemic preconditioning (RIPC) reduces renal injury in patients undergoing laparoscopic partial nephrectomy (LPN).
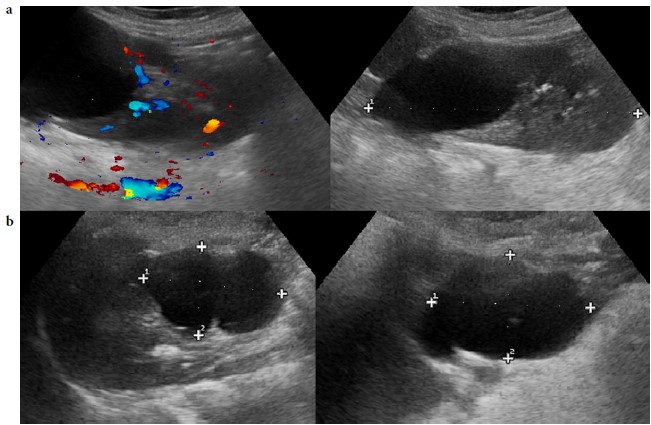
PATIENTS AND METHODS
• In all, 82 patients undergoing LPN were randomly assigned to either the RIPC or control group, with 40 and 38 patients, respectively completing 6-months follow-up.
• RIPC was conducted after induction of anaesthesia, which consisted of three 5-min cycles of right lower limb ischaemia and 5 min of reperfusion during each cycle.
• The primary outcome was the absolute change in glomerular filtration rate (GFR) of the affected kidney by renal scintigraphy from baseline to 6 months.
• The secondary outcomes included urinary retinol-binding protein (RBP) levels measured at 24 and 48 h, serum creatinine, and estimated GFR (eGFR) at 1 and 6 months, and changes in GFR by renal scintigraphy.
RESULTS
• There were no differences in the change of GFR of the affected kidney at 6 months, while it was significantly decreased by 15.0% in the control group vs 8.8% in the RIPC group at 1 month (P = 0.034).
• The urinary RBP levels increased 8.4-fold at 24 h in the control group compared with a lower increase of 3.9-fold in the RIPC group (P < 0.001).
• There were no differences in the serum creatinine level or eGFR at 1 and 6 months between the two groups.
CONCLUSIONS
• In patients undergoing LPN, RIPC using transient lower limb ischaemia may reduce renal impairment in the short term, but failed in the longer term despite a non-significant trend in favour of RIPC.
• These novel data support the need for a larger study of RIPC during LPN surgery.
Read Previous Articles of the Week
Editorial: Accepting the positive results of unconventional methods
It is sometimes difficult to accept the results of a study based on a concept that is unfamiliar, involves unknown physiological mechanisms, or shows results that defy rational explanation. Remote ischaemic preconditioning (RIPC) is probably not a familiar topic to most urologists and, admittedly, was not familiar to this reviewer until now. Yet the authors, based on animal models and clinical data from non-urological literature, conducted a prospective, surgeon and patient ‘blinded’, randomised controlled trial to evaluate the potential benefit of RIPC in minimising ischaemic damage. By most available factors affecting postoperative renal function (warm ischaemia time, tumour complexity as measured by Preoperative Aspects and Dimensions Used for an Anatomical [PADUA] scores, preoperative renal function, tumour stage, etc.), no difference existed between the control and study groups. The authors found that patients undergoing RIPC had a lower change in estimated GFR (eGFR) at 1 month and appeared to have less ischaemic damage based on urinary marker levels (retinol binding protein) and functional imaging parameters. Unfortunately, the short-term benefit of RIPC did not translate to improvements over a longer period, with no differences at 6 months or in absolute eGFR between the two groups.
The authors should be congratulated for conducting such an elegant trial, unfamiliar and unconventional as the concept may be. Strengths of this study include its randomised ‘blinded’ design, correlation with metabolite, urinary marker and imaging findings, 6-month follow-up, and due diligence for assessing most pre-analytic factors. Limitations include the absence of data on residual functioning renal parenchyma, which arguably is the single best predictor of function in an operated kidney; additionally, this population with outstandingly good renal function (≈120 mL/min/1.73 m2 in both groups) with very few comorbidities (<5–10% incidence of hypertension and diabetes) may not translate equally to the less healthy, more renally impaired Western population. The results may appear to be underwhelming, but I agree with the authors that further study is needed, and in particular for the Western population. The major impact from this reviewer’s perspective is for the patient with baseline renal compromise, whose risk for short- and long-term ischaemic renal injury is greater, and who could most benefit from a simple protective measure. Should we now enter unfamiliar territory and accept that the results of a randomised, ‘blinded’, prospective trial of a simple but unconventional method provide sufficient justification for testing this strategy in a higher risk population?
Surena F. Matin
Department of Urology, University of Texas MD Anderson Cancer Center, Houston, TX, USA
Video: Remote ischaemic preconditioning: good for the short term
Effect of remote ischaemic preconditioning on renal protection in patients undergoing laparoscopic partial nephrectomy: a ‘blinded’ randomised controlled trial
Jiwei Huang, YongHui Chen, Baijun Dong, Wen Kong, Jin Zhang, Wei Xue, DongMing Liu and Yiran Huang
Department of Urology, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
OBJECTIVE
• To evaluate whether remote ischaemic preconditioning (RIPC) reduces renal injury in patients undergoing laparoscopic partial nephrectomy (LPN).
PATIENTS AND METHODS
• In all, 82 patients undergoing LPN were randomly assigned to either the RIPC or control group, with 40 and 38 patients, respectively completing 6-months follow-up.
• RIPC was conducted after induction of anaesthesia, which consisted of three 5-min cycles of right lower limb ischaemia and 5 min of reperfusion during each cycle.
• The primary outcome was the absolute change in glomerular filtration rate (GFR) of the affected kidney by renal scintigraphy from baseline to 6 months.
• The secondary outcomes included urinary retinol-binding protein (RBP) levels measured at 24 and 48 h, serum creatinine, and estimated GFR (eGFR) at 1 and 6 months, and changes in GFR by renal scintigraphy.
RESULTS
• There were no differences in the change of GFR of the affected kidney at 6 months, while it was significantly decreased by 15.0% in the control group vs 8.8% in the RIPC group at 1 month (P = 0.034).
• The urinary RBP levels increased 8.4-fold at 24 h in the control group compared with a lower increase of 3.9-fold in the RIPC group (P < 0.001).
• There were no differences in the serum creatinine level or eGFR at 1 and 6 months between the two groups.
CONCLUSIONS
• In patients undergoing LPN, RIPC using transient lower limb ischaemia may reduce renal impairment in the short term, but failed in the longer term despite a non-significant trend in favour of RIPC.
• These novel data support the need for a larger study of RIPC during LPN surgery.