Video: T1 renal tumours: Partial versus Radical Nephrectomy
Partial versus Radical Nephrectomy for T1 renal tumours: An analysis from the British Association of Urological Surgeons Nephrectomy Audit
OBJECTIVES
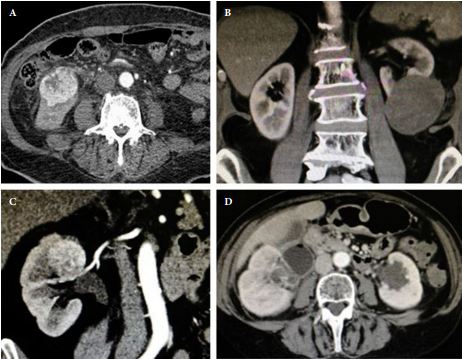
To analyse and compare data from the British Association of Urological Surgeons Nephrectomy Audit for perioperative outcomes of partial (PN) and radical nephrectomy (RN) for T1 renal tumours.
PATIENTS AND METHODS
UK consultants were invited to submit data on all patients undergoing nephrectomy between 1 January and 31 December 2012 to a nationally established database using a standard pro forma. Analysis was made on patient demographics, operative technique, and perioperative data/outcome between PN and RN for T1 tumours.
RESULTS
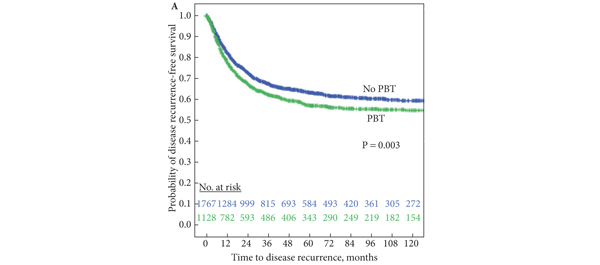
Overall, data from 6 042 nephrectomies were reported of which 1 768 were performed for T1 renal tumours. Of these, 1 082 (61.2%) were RNs and 686 (38.8%) were PNs. The mean age of patients undergoing PN was lower (PN 59 years vs RN 64 years; P < 0.001) and so was the WHO performance score (PN 0.4 vs RN 0.7; P < 0.001). PN for the treatment of T1a tumours (≤4 cm) accounted for 55.6% of procedures, of which 43.9% were performed using a minimally invasive technique. For T1b tumours (4–7 cm), 18.9% of patients underwent PN, in 33.3% of which a minimally invasive technique was adopted. The vast majority of RNs for T1 tumours were performed using a minimally invasive technique (90.3%). Of the laparoscopic PNs, 30.5% were robot-assisted. There was no significant difference in overall intraoperative complications between the RN and PN groups (4% vs 4.3%; P = 0.79). However, PN accounted for a higher overall postoperative complications rate (RN 11.3% vs PN 17.6%; P < 0.001). RN was associated with a markedly reduced risk of severe surgical complications (Clavien Dindo classification grade ≥3) compared with PN even after adjusting for technique (odds ratio 0.30; P = 0.002). Operation time between RN and PN was comparable (141 vs 145 min; P = 0.25). Blood loss was less in the RN group (mean for RN 165 vs PN 323 mL; P < 0.001); however, transfusion rates were similar (3.2% vs 2.6%; P = 0.47). RN was associated with a shorter length of stay (median 4 vs 5 days; P < 0.001). A direct comparison between robot-assisted and laparoscopic PN showed no significant differences in operation time, blood loss, warm ischaemia time, and intraoperative and postoperative complications.
CONCLUSIONS
PN was the method of choice for treatment of T1a tumours whereas RN was preferred for T1b tumours. Minimally invasive techniques have been widely adopted for RN but not for PN. Despite the advances in surgical technique, a substantial risk of postoperative complications remains with PN.