Papillary Renal Cell Carcinoma and Clear Cell Renal Cell Carcinoma Arising in a Single Kidney
We report a case of clear cell RCC and papillary RCC arising in the same kidney.
Authors: Tait, Laura; Coleman, Pamela; Ahaghotu, Chiledum
Corresponding Author: Tait, Laura Department of Surgery-Division of Urology, Howard University Hospital Washington, DC
Introduction
Renal cell carcinoma (RCC) is responsible for 80 percent of all primary renal neoplasms and approximately 65,000 Americans are diagnosed with RCC each year (1). Clear cell RCC comprises a majority of all RCC tumors diagnosed histologically. They arise from the proximal tubule and macroscopically appearsolid or cystic (2). Clear cell RCC occurs most commonly as a sporadic disease. Papillary RCC are diagnosed in 10 to 15 percent of patients with RCC (3, 4, 5, 6). As with clear cell cancers, papillary RCCs originate from the proximal tubule, but they are morphologically and genetically distinct malignancies. Papillary carcinomas are frequently multifocal and bilateral, and commonly present as small, early stage tumors (7). For localized disease, radical nephrectomy has been the most widely used approach and remains the preferred procedure for cases suggestive of renal malignancy. The diagnosis of clear cell RCC has been established by identifying distinct morphological and histologic features of this tumor following nephrectomy. These unique qualities include neoplastic cells with clear cytoplasm in an acinar growth pattern. These findings separate it from papillary RCC in which psammoma bodies and a strong positive staining for CK7 are characteristic. This case is unique in that there were no prior available reports describing two RCC tumors of separate origin found within a single kidney. We report a case of clear cell RCC and papillary RCC arising in the same kidney.
Case report
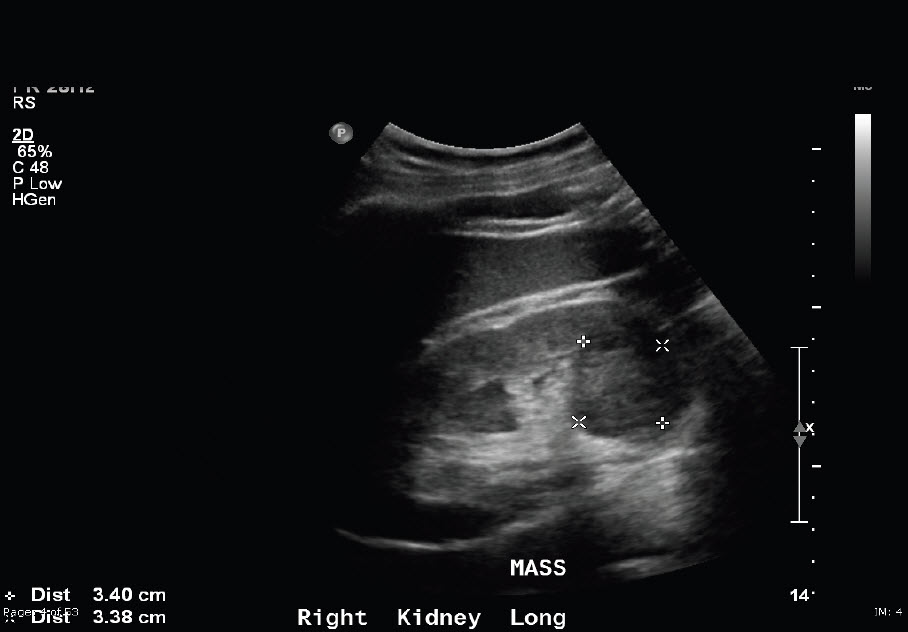
A 55-year-old African American male presented to his PCP with a two-week history of hematuria. The patient’s past medical history included hypertension, hepatitis c, and a hernia repair. He was referred to urology and a computed tomography scan demonstrateda complex heterogenous cyst within the right kidney with characteristics suggestive of malignancy and the presence of a left pelvic kidney. Right nephrectomy was performed. Two renal tumors were noted upon gross examination. The main tumor mass was a well-circumscribed, lobulated, homogeneous yellow tumor at the inferior pole of the kidney measuring 4.2×4.0x3.6 cm and demonstrated microscopic invasion of the renal sinus. The satellite tumor was found to be compressing the renal parenchyma at the inferior pole and was a 0.6 cm, firm, well-circumscribed nodule with homogeneous, tan/grey cut surface with characteristic hilar vessel wall invasion. Renal tumor tissues obtained at operation wasfixed in formalin and embedded in paraffin. The specimens were serially sectioned using three-micrometer thick cuts. The sections were stained with hematoxylin-eosin and immunohistochemical studies were undertaken. CK7 staining was performed with the satellite papillary renal cell carcinoma showing strong positive staining. CK7 staining was negative within the main tumor mass. The pathology results provide evidence that clear cell RCC and papillary RCC can simultaneously arise within a single kidney.
Pathology
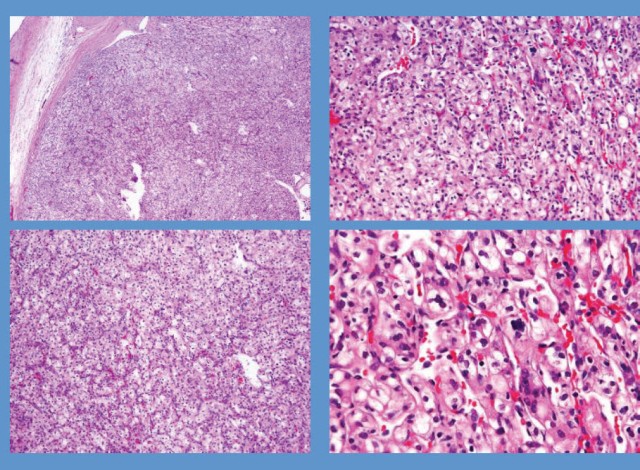
Macroscopically, the kidney showed no gross abnormalities. The tumor measuring 4.2 x 4.0 x 3.6 cm and the tumor measuring 0.6 cm were observed in the inferior pole. The cut surface of the main tumor showed a yellowish color while the satellite tumor had a tan/grey cut surface appearance. At the posterior/inferior pole it was noted that the renal capsule was expanded by a gelatinous blood clot. The cut surface is shown (Fig. 1).
Microscopically, the main tumor located at the inferior pole showed a proliferation of neoplastic cells with clear cytoplasm and an acinar growth pattern. The nuclear characteristics were a Fuhrman nuclear grade 4 (Fig. 2). Given this tumor’s microscopic characteristics, a diagnosis of clear cell carcinoma was made.
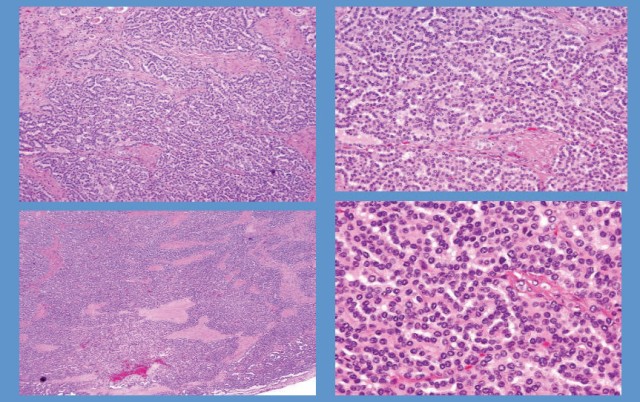
The satellite tumor showed a proliferation of neoplastic cells with foamy macrophages and psammoma bodies (Fig. 3). This satellite tumor also demonstrated strong positive staining for CK7, a well-known tumor marker for papillary renal cell carcinoma. Based on the microscopic and immunohistologic findings, a diagnosis of papillary renal cell carcinoma was made.
Discussion
This case report describes a unique finding of clear cell and papillary RCC within a single kidney. The pathology of this conditionis described to illustrate how both tumors were morphologically different from one another. This particular anomaly has not been previously described in the literature.
The risk factors for RCC have been well-documented and include smoking, hypertension, occupational exposure to toxic compounds, obesity, acquired cystic disease of the kidney, analgesic abuse nephropathy, and genetic predisposition (8,9). These documented findings are similar to our case report in that the patient had a history of hypertension. The literature suggests that hypertension predisposes to the development of RCC. Although our patient had high blood pressure for many years, the incidence of RCC seems to be independent of anti-hypertensive medications. Therefore, hypertension may have played a role in the development of clear cell and papillary RCC seen in this patient.
Another risk factor our patient had for developing RCC waschronic hepatitis c infection. An epidemiologic study of over 67,000 patients found that chronic infection with the hepatitis C virus was associated with a significantly increased risk of RCC (10). This risk factor combined with hypertension may have put our patient at increased risk for RCC.
Although no clear cell RCC and papillary RCC have been found simultaneously before, a coexisting RCC can be identified in 10 to 32 percent of patients with oncocytoma (11). This evidence demonstrates that two unique RCC tumors can exist in a single kidney. Our findings of two RCC within the same kidney is consistent with past evidence of simultaneous tumors but are new in that none have reported clear cell and papillary RCC. Therefore, in our case, we were able to determine the possible risk factors predisposing our patient to RCC and report the new discovery of two RCC tumors within the same kidney.
Conclusions
We present a unique example of clear cell and papillary RCC within the same kidney. Histology of the tissues at the time of nephrectomy confirmed the diagnosis of two distinct renal tumors. Risk factors for RCC seen in this patient include hypertension and chronic hepatitis c. Although there are reports of oncomytoma and coexisting RCC, there have been no observed findings of clear cell and papillary RCC simultaneously.
Fig. 1
Fig. 2
Fig.3
Image 1
References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62:10.
2. Presti JC Jr, Rao PH, Chen Q, et al. Histopathological, cytogenetic, and molecular characterization of renal cortical tumors. Cancer Res 1991; 51:1544.
3. Tannenbaum M. Ultrastructural pathology of human renal cell tumors.PatholAnnu 1971; 6:249.
4. Thoenes W, Störkel S, Rumpelt HJ. Histopathology and classification of renal cell tumors (adenomas, oncocytomas and carcinomas).The basic cytological and histopathological elements and their use for diagnostics.Pathol Res Pract 1986; 181:125.
5. Störkel S, van den Berg E. Morphological classification of renal cancer. World J Urol 1995; 13:153.
6. Patard JJ, Leray E, Rioux-Leclercq N, et al. Prognostic value of histologic subtypes in renal cell carcinoma: a multicenter experience. J ClinOncol 2005; 23:2763.
7. Beck SD, Patel MI, Snyder ME, et al. Effect of papillary and chromophobe cell type on disease-free survival after nephrectomy for renal cell carcinoma. Ann SurgOncol 2004; 11:71.
8. Mandel JS, McLaughlin JK, Schlehofer B, et al. International renal-cell cancer study. IV. Occupation. Int J Cancer 1995; 61:601.
9. Wolk A, Gridley G, Niwa S, et al. International renal cell cancer study. VII. Role of diet. Int J Cancer 1996; 65:67.
10. Gordon SC, Moonka D, Brown KA, et al. Risk for renal cell carcinoma in chronic hepatitis C infection. Cancer Epidemiol Biomarkers Prev 2010; 19:1066.
11. Chao DH, Zisman A, Pantuck AJ, et al. Changing concepts in the management of renal oncocytoma. Urology 2002; 59:635.
Date added to bjui.org: 12/12/2012
DOI: 10.1002/BJUIw-2012-060-web