Editorial: Is choline-based PET imaging still relevant in recurrent prostate cancer?
The search for the ideal imaging method to detect small metastatic deposits has largely remained elusive in the field of prostate cancer. However, functional positron emission tomography (PET)/CT is now guiding us in different directions. 11C-acetate PET/CT imaging was one of the first molecular imaging probes showing promise in clinical studies, along with 11C-choline, and more recently challenged by 68Ga-prostate-specific membrane antigen (PSMA) PET/CT [1-3]. So against this background, what does this new study by Esch et al. [4] presented here offer us?
Let us rewind and focus on where molecular imaging may have an impact in prostate cancer. In primary staging, the potential to accurately identify oligometastatic disease or even widespread metastatic disease before primary gland treatment is clearly advantageous. It can allow for wider treatment fields (extended lymphadenectomy or radiation fields), directed treatment of oligometastatic disease, placement into appropriate cytoreductive trials, and in some instances consideration of the use of earlier chemo-hormonal therapy. This study did not address this important clinical scenario [4]. Nor did it focus on primary diagnosis, another ‘holy grail’ for imaging more recently dominated by MRI [5].
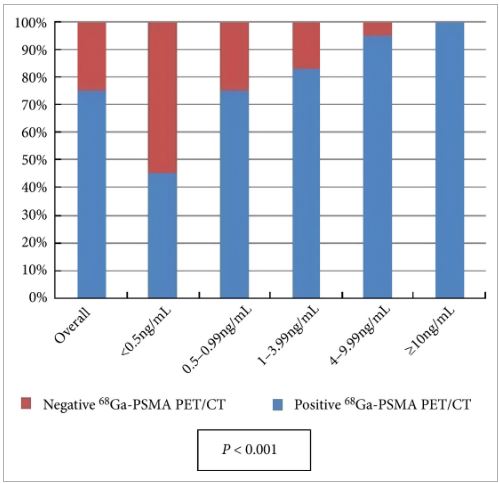
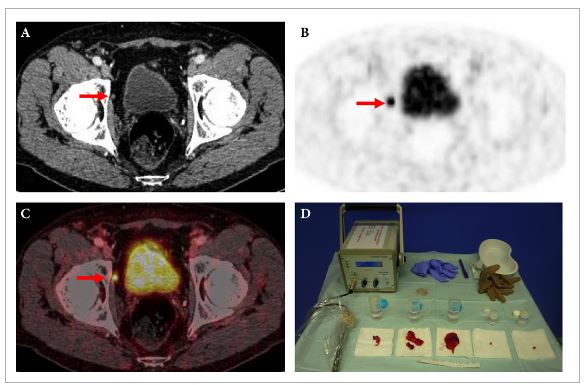
The clinical question addressed in this study was whether 11C-acetate PET is able to detect distant metastatic disease in men with PSA relapse after having undergone radical prostatectomy or prostate bed radiotherapy [4]. In other words, if distant metastatic disease is found then prostate bed radiation may be futile, although this assumption has not been subjected to high quality trials, but would seem logical. Also, in the era of oligometastatic disease, treatment (surgery and/or radiation) may be directed at nodal and other deposits to prolong time of systemic therapy such as androgen-deprivation therapy. So what is the ‘sweet spot’? Some would state for men having undergone surgery a PSA level of 0.2 ng/mL places the patient at risk of recurrence, although in clinical practice the level at which investigations are warranted can be as high as 1.0 ng/mL. This study found 11C-acetate PET had few positive results below a PSA level of 1.0 ng/mL. This is in contrast to a recent meta-analysis of 68Ga-PSMA PET/CT reporting positive studies at PSA levels of ≤0.2 ng/mL in 42% of patients [6].
The other group studied the detection of recurrent disease in men having undergone primary radiotherapy, although the numbers were low (six patients). We know this group of men are often undertreated for salvage treatment, and frequently placed on hormonal therapy. Again, early knowledge of locoregional or distant recurrence is required to allow best case selection and thus avoid futile salvage surgery, and also to know who may benefit from salvage lymphadenectomy and treatment of distant oligometastatic disease, if required.
The false-positive rate result for 11C-acetate PET/CT of 24% is notable and concerning. This may lead to unnecessary intervention, or even withholding prostate bed radiation that may have been of benefit. In contrast the false-positive rate for 11C-choline and 68Ga-PSMA PET/CT is far lower, although false-positive PSMA studies may occur in benign conditions and non-prostate cancer tumours.
It should be acknowledged that a strength of this study was comparative histology in a proportion of patients, allowing true sensitivity and specificity to be determined [4]. This is important information, as it guides correct decision-making, and such information is lacking for many other prostate cancer imaging probes, including 68Ga-PSMA, where these data are urgently required.
Overall, this study is important and adds to the rich milieu of available molecular imaging data on staging of possible recurrent or metastatic prostate cancer to date [4]. Current prospective trials exploring 11C-choline, 18F-FACBC (anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid), 18F-choline and 68Ga-PSMA with MRI and clinical outcomes should provide further insight into the most appropriate molecular imaging technique for staging prostate cancer.