In science, reports showing data deviating from what is expected are called anomalous observations. Metabolic syndrome (MetS) is a promoter of cancer at almost all sites [1]; however, when it comes to prostate cancer (PCa), a series of reports have been published showing an inverse relationship between MetS and its aspects and incident PCa. This lack of coherence in cancer research seriously hampers efforts to fight cancer disorders. It is therefore crucial to find an explanation for this incoherence.
In the search for a reasonable explanation for this anomalous observation, a hypothesis has been formulated, based on the study by Häggström et al. [2], and stating that the PSA-driven diagnostic procedure in PCa, which creates low-stage incident PCa material, is the culprit. The PSA-driven diagnostic procedure introduces several bias mechanisms, which tend to protect men with MetS from being diagnosed with PCa. Thus, men with MetS and its aspects are under-represented in PCa populations generated by PSA-driven diagnostics, thereby creating a distorted incident PCa population. This hypothesis also predicts that high-stage PCa, as well as non-localized and lethal PCa, are not subject to these bias mechanisms, as a minor reduction in the PSA level is of no importance for the PCa diagnosis at these high PSA levels. Finally, the hypothesis predicts that the link between MetS and incident PCa is stage-dependent. A study testing this hypothesis is now in progress.
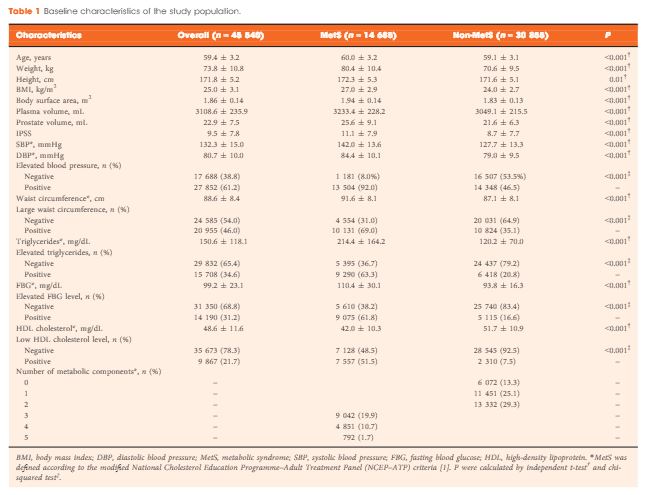
Several studies have reported that men with MetS had lower PSA levels compared with men without MetS. Zhao et al. [3] address this specific question in this issue of BJUI and confirm that the presence of MetS was independently associated with a lower PSA level and that the enlarged prostate gland, which is an aspect of MetS, partly concealed an even greater PSA level reduction [3]. The findings indicate that a bias mechanism inverses the link between MetS and incident PCa and support the above-mentioned hypothesis.
In short, the following bias mechanisms have been described. MetS is associated with greater body fat with increased aromatase activity, resulting in a reduced testosterone level, which, in turn, is related to a reduced PSA level, as the production of PSA is under androgen control. Another possible bias mechanism, leading to men with MetS being diagnosed less often with PCa, is that these men are more likely to be obese. It is well established that men with a higher BMI also have larger plasma volumes and therefore have greater haemodilution of the PSA production, resulting in a lower PSA level. This means that incident PCa is diagnosed less often in men with MetS, as their PSA level is lower. MetS is also associated with an enlarged prostate gland volume, which means that fewer incident PCas are diagnosed, given the same tumour volume and the same number of biopsies. Another bias mechanism is that a high proportion of men with high socio-economic status undergo PSA testing in the PSA era. It is well established that men with a high socio-economic status have a lower prevalence of MetS and therefore have higher PSA levels, as indicated by the present report in the BJUI [3], and an elevated risk of PCa. Thus, multiple bias mechanisms seem to conceal low-stage PCa in the PSA era.
If it could be confirmed that the negative relationship between MetS and incident PCa is a spurious observation as a result of bias mechanisms, this would open the door for the MetS hypothesis regarding the promotion of multiple cancer disorders. This door has previously been closed by findings in a series of reports of an inverse relationship between MetS and its aspects and incident prostate cancer. Furthermore, this could lead to increased efforts to fight the metabolic aberrations of MetS. It is now well established that MetS and its aspects could be reduced by changes in lifestyle, including physical activity and diet. The most convincing evidence of the effect of diet on MetS comes from studies involving decreased intake of carbohydrates and increased intake of unsaturated fats. Recently, leading authorities in nutrition, endocrinology and metabolism presented a critical review and concluded that carbohydrate restriction is the single most effective intervention to reduce all features of MetS [4]. Another review concluded that carbohydrate restriction is one of the few common interventions that target all features of MetS [5]. This conclusion has recently been confirmed in a meta-analysis by Mansoor et al. [6].
In conclusion, new knowledge challenges the anomalous observation of PCa showing a negative relationship between MetS and PCa. The credibility of the hypothesis that MetS is an important promoting factor for cancer at almost all sites is strengthened. MetS could be treated effectively with a low carbohydrate and high fat diet.
Jan Hammarsten, MD, PhD
Department of Urology, Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden
References
2Haggstrom C, Stocks T, Ulmert D et al. Prospective study on metabolic factors and risk of prostate cancer. Cancer 2012; 118: 6199–206
3 Zhao S, Xia M, Tang J et al. The actual lowering effect of metabolic syndrome on serum prostate-specific antigen levels is partly concealed by enlarged prostate: results from large-scale population-based study. BJU Int 2017; 120: 482–9
4 Feinman RD, Pogozelski WK, Astrup A et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 2015;31: 1–13
5 Accurso A, Bernstein RK, Dahlqvist A et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: time for critical appraisal. Nutrition & Metabolism 2008; 5: 9
6 Mansoor N, Vinknes UJ , Veierod MB et al. Effects of low-carbohydrate diets v. low fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Br J Nutrition 2016; 115: 466–7