The new AUA PSA Testing Guidelines leave me scratching my head
 The fact that Otis Brawley describes the new PSA testing guidelines of the American Urological Association (AUA) as “wonderful”, should immediately raise a red flag at AUA headquarters. Dr Brawley, Chief Medical Officer of the American Cancer Society, and the most vocal anti-prostate cancer screening voice in the USA over the past decade, has enthusiastically welcomed the new document and “commended” the AUA for bringing its policy closer to that of his Society. The Guidelines have also been compared to those of the United States Preventative Services Task Force (USPSTF) which completely opposes PSA testing in any situation – a position which the AUA called “inappropriate and irresponsible” just a few months ago. Oh dear – where has it all gone wrong? ?
The fact that Otis Brawley describes the new PSA testing guidelines of the American Urological Association (AUA) as “wonderful”, should immediately raise a red flag at AUA headquarters. Dr Brawley, Chief Medical Officer of the American Cancer Society, and the most vocal anti-prostate cancer screening voice in the USA over the past decade, has enthusiastically welcomed the new document and “commended” the AUA for bringing its policy closer to that of his Society. The Guidelines have also been compared to those of the United States Preventative Services Task Force (USPSTF) which completely opposes PSA testing in any situation – a position which the AUA called “inappropriate and irresponsible” just a few months ago. Oh dear – where has it all gone wrong? ?
For those who haven’t yet seen the document, here are the five statements issued by the Guideline committee at the Annual Meeting of the AUA in San Diego this week along with some of my thoughts in italics:
- The Panel recommends against PSA screening in men under age 40 years. This appears reasonable.
- The Panel does not recommend routine screening in men between ages 40 to 54 years at average risk. I have some problems with this (as do many others). In addition to this statement, the AUA highlights its view that the likelihood of causing harm is high and that any benefit is marginal. It appears to have completely dismissed evidence (and its own previous view), that a baseline PSA in men in this age group is highly predictive of future prostate cancer, metastasis and death. In my view, there is considerable value in having a baseline PSA in this age group and I am disappointed that the AUA has not recognised the evidence to support this.
- For men ages 55 to 69 years the Panel recognizes that the decision to undergo PSA screening involves weighing the benefits of preventing prostate cancer mortality in 1 man for every 1,000 men screened over a decade against the known potential harms associated with screening and treatment. For this reason, the Panel strongly recommends shared decision-making for men age 55 to 69 years that are considering PSA screening, and proceeding based on a man’s values and preferences. I agree with the emphasis here on shared decision-making, although the concept can be somewhat nebulous and difficult to achieve in real-life. However, I think that this statement somewhat over-emphasises the harms associated with PSA testing in this group. Rather than portray the reduction in prostate cancer mortality as being very minor (1 in 1000), men should know that when compared with a man who chooses not to have PSA testing in this age group, those who do have regular PSA testing have a 44% reduction in prostate-cancer mortality over a 14 year period. Furthermore, the numbers needed to screen (293) and number needed to treat (12) to save one life stack up very well when compared with other screening modalities such as mammography (Hugosson et al). Why has the AUA instead chosen to over-emphasise the harms? This is disappointing.
- To reduce the harms of screening, a routine screening interval of two years or more may be preferred over annual screening in those men who have participated in shared decision-making and decided on screening. As compared to annual screening, it is expected that screening intervals of two years preserve the majority of the benefits and reduce over-diagnosis and false positives. This appears reasonable.
- The Panel does not recommend routine PSA screening in men over age 70 years or any man with less than a 10 to 15 year life expectancy. Yes, but this strong advice not to offer PSA testing in men greater than 70 belies the fact that many men in this age group have a long life expectancy (eg in Australia a male who reaches 70 has a 15 year life expectancy (www.abs.gov.au), and an early diagnosis of prostate cancer may prevent their untimely death from this disease. Clearly, not all men in their 70’s are the same but following this advice to the letter could deny many men the option of avoiding death from prostate cancer in later life.
Therefore, it appears that the only circumstances under which the AUA currently recommend a PSA test be performed is for men between the age of 55 and 69 following a weekend seminar so they can be adequately informed (or thoroughly confused).
These statements have led to headlines such as these in the mass media today:
- Urology Group Stops Recommending Routine PSA Test (USA Today)
- Looser Guidelines Issued on Prostate Cancer Screening (New York Times)
- Urologists No Longer Support Routine Prostate Cancer Screening (Minn Post)
- Most men don’t need PSA test (Arizona Star)
- AUA No Longer Recommend Routine PSA Testing For Prostate Cancer (Huff Post)
I think it is reasonable to say that this AUA document adds more confusion than clarity to the debate around prostate cancer testing. It has certainly provoked some anger among prominent members of the AUA who voiced their displeasure to the Committee during the plenary and also through social media. Dr Catalona was first to the microphone asking why AUA members were not more widely consulted prior to publication and in particular, challenging the guidance around men aged 40-54 (reported on Twitter):
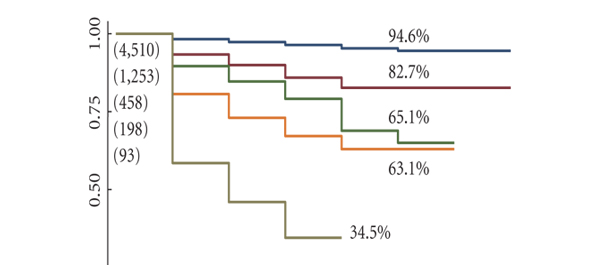
Much progress has been made in the last few decades with a 30% reduction in prostate cancer-specific mortality since the introduction of PSA testing. And while we accept that this has led to a large amount of over-treatment of less aggressive disease, it is clear that (at least outside the USA), active surveillance is being enthusiastically embraced for appropriate patients. Any return towards the pre-PSA era would likely lead to a reversal in these mortality gains and we would again see many more men presenting to our rooms with incurable disease.
As Dr Smith editorialized in the Journal of Urology following the publication of the ERSPC and PLCO trials in 2009, “Treatment or non-treatment decisions can be made once a cancer is found, but not knowing about it in the first place surely burns bridges”. It is clear that many urologists consider these new AUA PSA Guidelines to be in danger of burning these bridges. However, rather than burn bridges, it is likely that urologists and others will ignore these guidelines and continue to counsel men in a more balanced fashion about the pros and cons of PSA testing. The AUA will then need to consider whether ignored guidelines are failed guidelines.
Prof Tony Costello is a Director and Professor of Urology at the Royal Melbourne Hospital, Melbourne, Australia.
Twitter: @proftcostello
Comments on this blog are now closed.