Video: Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques
Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques in oncology: analysis of English secondary care data for radical prostatectomy and partial nephrectomy
Objectives
To evaluate postoperative health resource utilisation and secondary care costs for radical prostatectomy and partial nephrectomy in National Health Service (NHS) hospitals in England, via a comparison of robot-assisted, conventional laparoscopic and open surgical approaches.
Patients and Methods
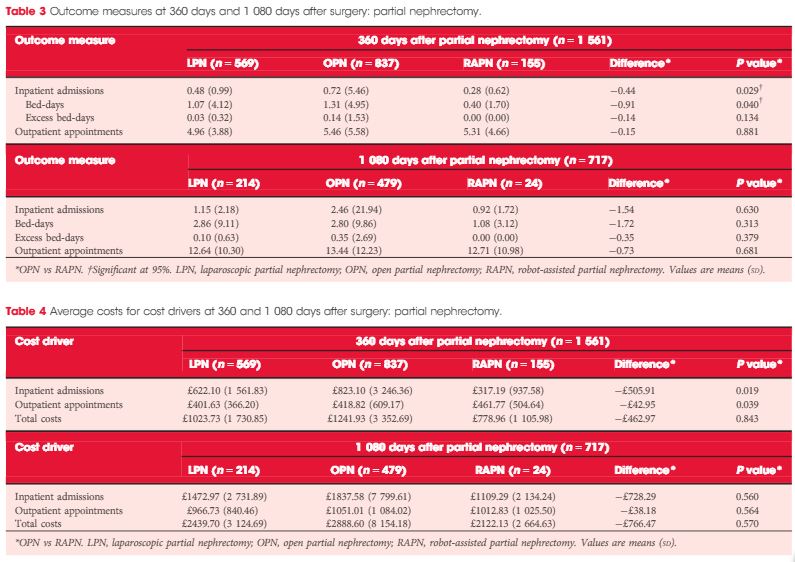
We retrospectively analysed the secondary care records of 23 735 patients who underwent robot-assisted (RARP, n = 8 016), laparoscopic (LRP, n = 6 776) or open radical prostatectomy (ORP, n = 8 943). We further analysed 2 173 patients who underwent robot-assisted (RAPN,n = 365), laparoscopic (LPN, n = 792) or open partial nephrectomy (OPN, n = 1 016). Postoperative inpatient admissions, hospital bed-days, excess bed-days and outpatient appointments at 360 and 1 080 days after surgery were reviewed.
Results
Patients in the RARP group required significantly fewer inpatient admissions, hospital bed-days and excess bed-days at 360 and 1 080 days than patients undergoing ORP. Patients undergoing ORP had a significantly higher number of outpatient appointments at 1 080 days. The corresponding total costs were significantly lower for patients in the RARP group at 360 days (£1679 vs £2031 for ORP; P < 0.001) and at 1 080 days (£3461 vs £4208 for ORP; P < 0.001). In partial nephrectomy, Patients in the RAPN group required significantly fewer inpatient admissions and hospital bed-days at 360 days compared with those in the OPN group; no significant differences were observed in outcomes at 1 080 days. The corresponding total costs were lower for patients in the RAPN group at 360 days (£779 vs £1242 for OPN,P = 0.843) and at 1 080 days (£2122 vs £2889 for ORP; P = 0.570). For both procedure types, resource utilisation and costs for laparoscopic surgeries lay at the approximate midpoint of those for robot-assisted and open surgeries.
Conclusion
Our analysis provides compelling evidence to suggest that RARP leads to reduced long-term health resource utilisation and downstream cost savings compared with traditional open and laparoscopic approaches. Furthermore, despite the limitations that arise from the inclusion of a small sample, these results also suggest that robot-assisted surgery may represent a cost-saving alternative to existing surgical options in partial nephrectomy. Further exploration of clinical cost drivers, as well as an extension of the analysis into subsequent years, could lend support to the wider commissioning of robot-assisted surgery within the NHS.