Surgery or Radiation in Prostate Cancer?
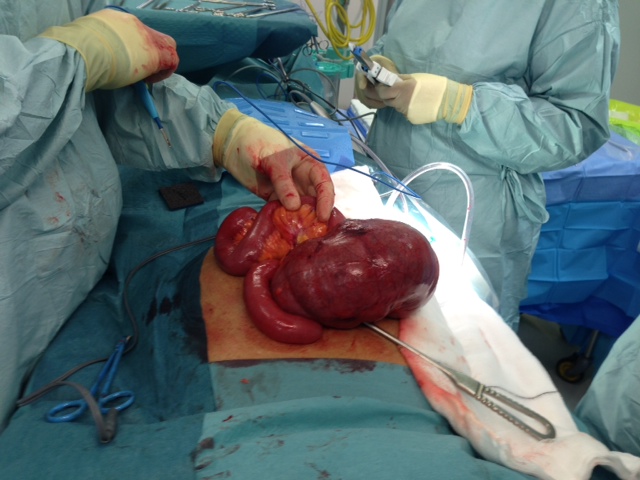
 I am sure many of you are familiar with the clinical situation I see every week of a man with newly-diagnosed prostate cancer asking me about his options. While we steer many men with low risk prostate cancer towards surveillance nowadays, for those with intermediate or high risk disease intervention is usually their best option, especially if they have a long life expectancy. This gives us the dilemma of whether to recommend surgery or radiotherapy.
I am sure many of you are familiar with the clinical situation I see every week of a man with newly-diagnosed prostate cancer asking me about his options. While we steer many men with low risk prostate cancer towards surveillance nowadays, for those with intermediate or high risk disease intervention is usually their best option, especially if they have a long life expectancy. This gives us the dilemma of whether to recommend surgery or radiotherapy.
In Oxford, we have a long and pioneering history of evidence-based medicine, and I lament the lack of RCTs in this field. The only one, ProtecT, which is being led also by Oxford, will not report before 2016, and will at least in part be subject to volunteer bias. Now, the question of surgery or radiotherapy for prostate cancer is not a new question. Millions of men have undergone these treatments across the globe and over the decades, and many other investigators have evaluated this question.
Most of these previous studies suggest that surgery in indeed superior but the main problem with them is inadequate control for selection bias (what we term in the trade as confounding by indication) – i.e. that men undergoing surgery are fitter and have better prognosis from their cancer point of view than men undergoing radiotherapy, and thus it’s not a fair comparison. Another problem with these previous studies is that the datasets used are not very comprehensive – not all men are included, and we don’t know all their important risk factors. All this makes it difficult to be confident in their results.
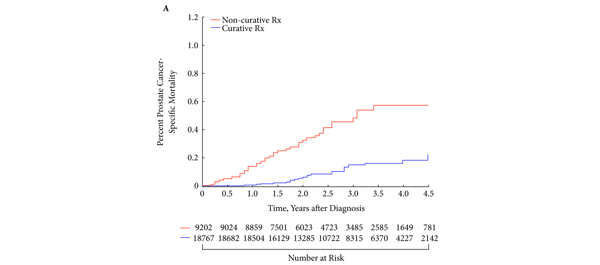
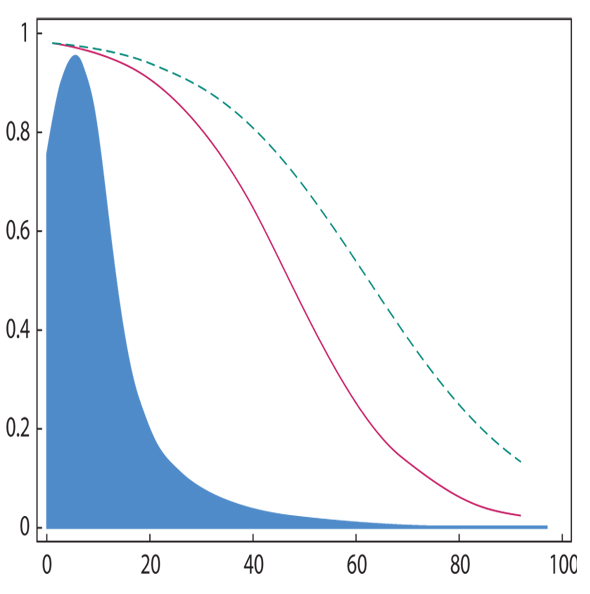
What is different about the BMJ study (https://www.bmj.com/content/348/bmj.g1502) is that the dataset and the statistics were top-notch. More than 98% of men diagnosed with prostate cancer in Sweden from 1998 onwards were included, and virtually all important data points were recorded with <2% incomplete data. Men were followed for up to 15 years and 4 different sets of statistical models were done to balance the surgery and radiotherapy groups with each other.
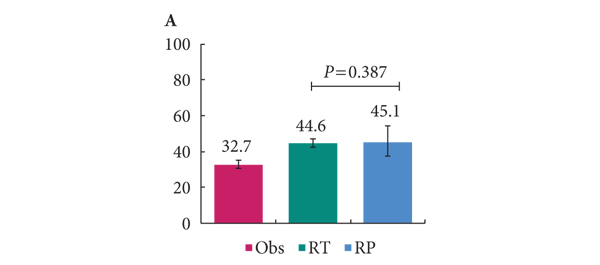
Remarkably, all sets of models came up with the same answer: that surgery led to better survival results than radiotherapy, especially for the men with intermediate and high risk prostate cancer and even more so if they had a long life expectancy. If I were a barrister, I would say this study provides strong evidence to build the case that surgery is a better option in survival terms for the majority of men who need treatment for localized prostate cancer. Medicine, like law, is never about absolutes, it’s about risk and probability. Can I prove that surgery is better than radiotherapy from this study – no; but there certainly seems a strong case to argue.
The current BJUI Article of the Week is another excellent article on the same subject (https://www.bjuinternational.com/article-of-the-week/prostate-cancer-sun-shines-light-on-surgical-survival/)
You can download Drs Sooriakumaran & Wiklund’s slideshow on their article by clicking here (1.5mb)
Prasanna Sooriakumaran is a robotic prostate & bladder cancer surgeon and academic at Oxford and Karolinska. @PSooriakumaranu