Posts
In search of the ROSETTA stone (again)?
We are having an amazing year of scientific discovery in our specialty. 2016 has already seen the results of the only randomised trial comparing open versus robotic radical prostatectomy from Australia and the ProtecT trial from UK discussed intensively on Blogs@BJUI. The PROMIS of MRI is expected to change the practice of prostate biopsies in response to a raised PSA. The teams completing these trials deserve our heartiest congratulations as it is well known how difficult randomised trials in surgery are to initiate and complete.
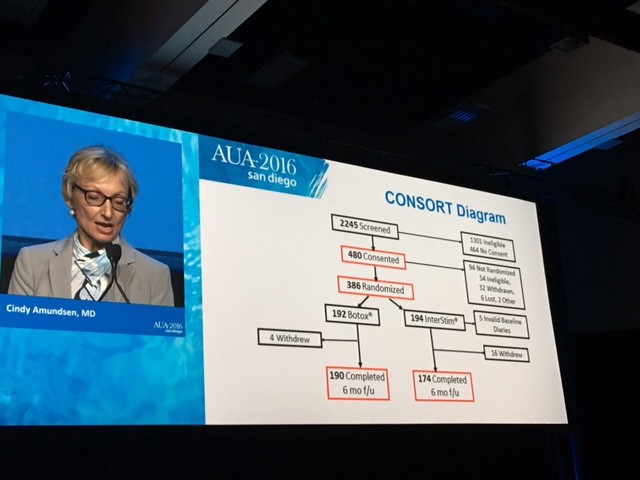
As if this was not enough, this month the randomised controlled trial comparing Botox (Onabotulinum toxin A) to Interstim (sacral neuromodulation) in patients with refractory overactive bladder has been reported in JAMA. It is otherwise known as the ROSETTA study (Refractory Overactive Bladder: Sacral NEuromodulation v. BoTulinum Toxin Assessment).
This is an example of what collaboration between individuals and teams within a pelvic floor group can achieve. Cindy Amundsen, the lead author, presented the trial results at the #AUA16 late breaking abstract session in San Diego.
The CONSORT diagram is shown here
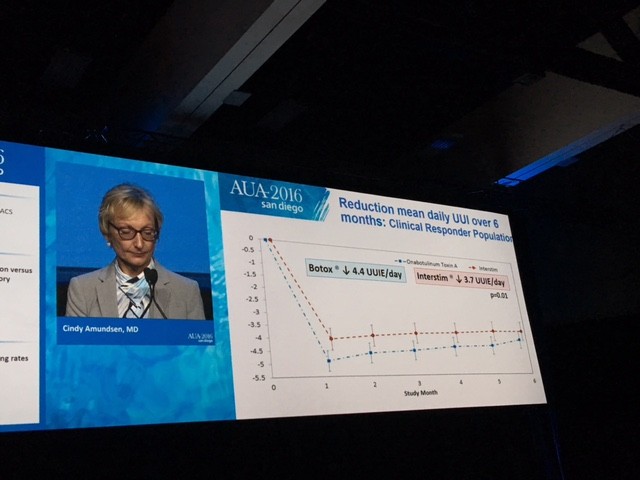
The primary outcome measure showing Botox winning over Interstim (narrowly) in reducing urgency urinary incontinence is demonstrated in this diagram.
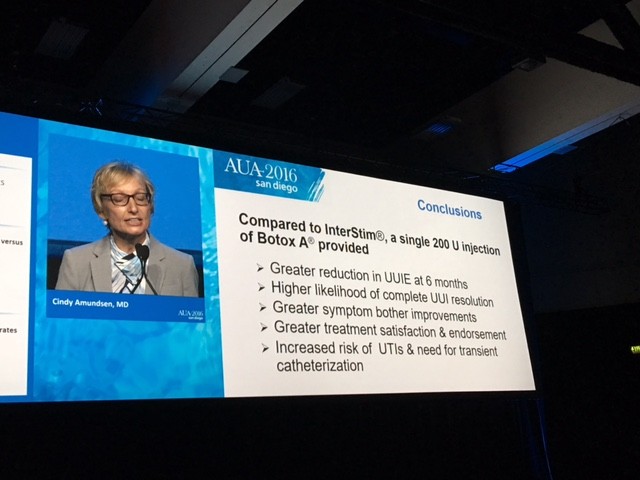
The summary results are shown here
So what would you do for your patient with refractory overactive bladder who has failed Anticholinergics and Mirabegron?
I have spent the last week thinking about the trial results carefully and was asked exactly this question at the International Endourology Forum in China. There are a number of important aspects to consider. The dose of Botox used in the trial was 200 units while the licensed dose is 100 units for overactive bladder of non-neurogenic origin. We know that one size does not fit all and indeed some patients failing 100 units need higher doses of Botox. It remains unknown as to what would have happened if 100 units of Botox was compared to Interstim as the authors are quite guarded about their own conclusions about the benefits.
The side effects also need to be carefully discussed with the patient. The UTI rate in the Botox group is about three times that of the Interstim group. Most patients may accept a period of oral antibiotics to counter this. The risk of CISC dropped from 8% at 1 month to 2% at 6 months in the Botox group. This is lower than previously reported in Phase lll studies. The need for revision or removal in the Interstim patients was around 3% – small but not to be ignored.
Punchline
If I was the patient in question, I would have Botox initially, preserving Interstim for later. It is less invasive and can be repeated roughly once a year if needed. Call me “lilly livered” but I do not like the idea of having a little box, however tiny, inside my bum and occasionally having to sit on it! I look forward to the smarter new generation of minimally invasive or even non-invasive nerve stimulators. But then it would need another randomised trial, many years of unanswered questions, perhaps even wastage of a lot of grant money…………..yawn!!
In the meantime, I will take my chances with Botox and counsel my patients accordingly. Unlike the famous ROSETTA stone, the key to understanding the mystery behind hieroglyphs and the controversy as to whether it should at all be in the British museum, I fail to see any such controversy with this nice trial in JAMA.
My thoughts and message are clear. Are yours?
Article of the Month: Gleason Grading in the Spotlight
Every Month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Klaus Brasso, discussing his paper.
If you only have time to read one article this week, it should be this one.
The impact of the 2005 International Society of Urological Pathology consensus guidelines on Gleason grading – a matched pair analysis
Objectives
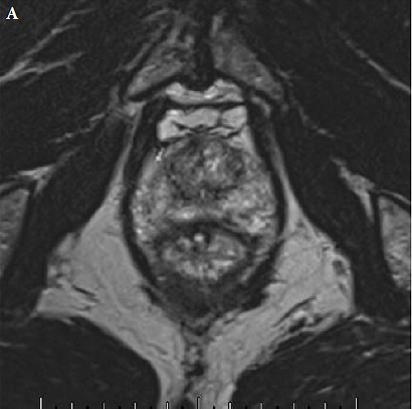
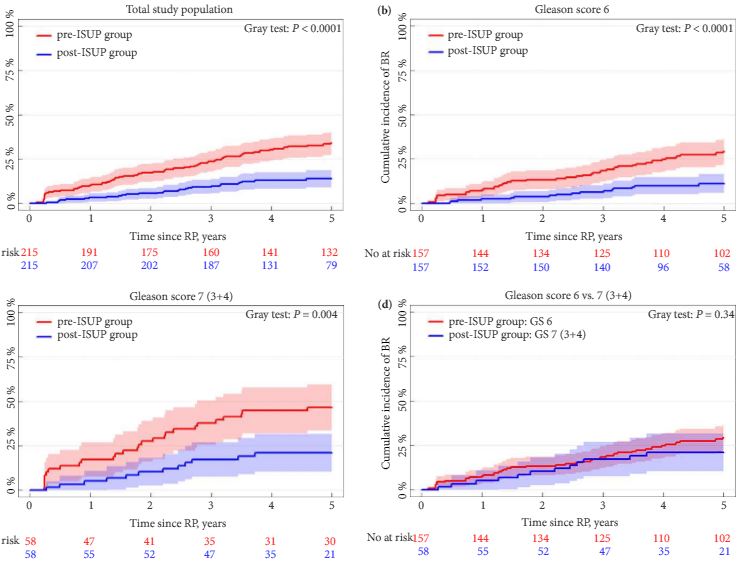
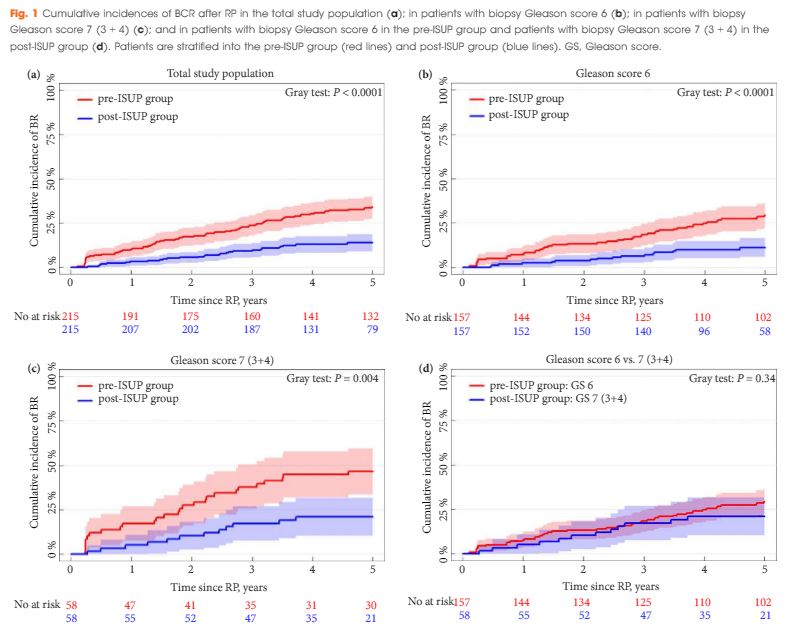
To investigate whether the International Society of Urological Pathology (ISUP) 2005 revision of the Gleason grading system has influenced the risk of biochemical recurrence (BCR) after radical prostatectomy (RP), as the new guideline implies that some prostate cancers previously graded as Gleason score 6 (3 + 3) are now considered as 7 (3 + 4).
Patients and methods
A matched-pair analysis was conducted. In all, 215 patients with Gleason score 6 or 7 (3 + 4) prostate cancer on biopsy who underwent RP before 31 December 2005 (pre-ISUP group), were matched 1:1 by biopsy Gleason score, clinical tumour category, PSA level, and margin status to patients undergoing RP between 1 January 2008 and 31 December 2011 (post-ISUP group). Patients were followed until BCR defined as a PSA level of ≥0.2 ng/mL. Risk of BCR was analysed in a competing-risk model.
Results
The median follow-up was 9.5 years in the pre-ISUP group and 4.8 years in the post-ISUP group. The 5-year cumulative incidences of BCR were 34.0% and 13.9% in the pre-ISUP and post-ISUP groups, respectively (P < 0.001). The difference in cumulative incidence applied to both patients with Gleason score 6 (P < 0.001) and 7 (3 + 4) (P = 0.004). There was no difference in the 5-year cumulative incidence of BCR between patients with pre-ISUP Gleason score 6 and post-ISUP Gleason score 7 (3 + 4) (P = 0.34). In a multiple Cox-proportional hazard regression model, ISUP 2005 grading was a strong prognostic factor for BCR within 5 years of RP (hazard ratio 0.34; 95% confidence interval 0.22–0.54; P < 0.001).
Conclusion
The revision of the Gleason grading system has reduced the risk of BCR after RP in patients with biopsy Gleason score 6 and 7 (3 + 4). This may have consequences when comparing outcomes across studies and historical periods and may affect future treatment recommendations.
Editorial: Current Gleason score 3 + 4 = 7: has it lost its significance compared with its historical counterpart?
Berg et al. [1] report that patients classified as Gleason score 7 (3 + 4) according to the revised grading system published in 2005 are to some extent similar to patients with pre-2005 Gleason score 6, at least in terms of risk of biochemical recurrence. The logical but not necessarily correct conclusion is that current patients with Gleason score 7 on biopsy are appropriate candidates for active surveillance.
What must be kept in mind is that, using the post-2005 revised grading system, approximately 25% of men with Gleason score 3 + 4 = 7 on biopsy have either 3 + 4 = 7 with tertiary pattern 5 or >4 + 3 = 7 in the corresponding radical prostatectomy [1]. With the exception of men with a limited life expectancy, these men need definitive therapy for their potentially life-threatening cancer. Numerous studies have shown that extended biopsies, whether they are >10- or 12-core, are associated with less upgrading than sextant biopsies [2]. In the report by Berg et al. [1], the median number of cores sampled before 2005 was 6 with an interquartile range (IQR) of 6–6 compared with a median (IQR) of 10 (10–12) cores after 2005. Consequently, in their cohorts, the pre-2005 group of men with Gleason score 3 + 3 = 6 were more likely to have unsampled higher grade cancer and a correspondingly worse prognosis more closely approximating post-2005 better-sampled Gleason score 3 + 4 = 7 cancers.
Berg et al. [1] further claim that the prognostic and clinical value of Gleason score 7 has been weakened since the 2005 modifications. In fact, the revised grading system more accurately reflects prostate cancer biology than the pre-2005 Gleason system. The major consequence of the modification, as Berg et al. [3] illustrate, has been the better prognosis associated with post-2005 Gleason score 6 cancer because patterns associated with more aggressive behaviour have been shifted to Gleason score 7. Historically, a diagnosis of Gleason score 6 cancer, even at radical prostatectomy, was not as predictive of ‘good’ behaviour, and had a higher rate of progression with some men even dying from prostate cancer [4]. Currently, Gleason score 6 cancer at radical prostatectomy has a 96% cure rate at 5 years, even including cases with extraprostatic extension and positive margins [3]. Several studies have shown that post-2005 pure Gleason score 6 cancers at radical prostatectomy are incapable of metastasizing to lymph nodes [4]. Berg et al. are correct, however, that men with a post-2005 grade of Gleason Score 3 + 4 = 7 have a better prognosis than those graded prior to 2005. As a consequence, it has been recommended that pathologists should record the percent pattern 4 in cases with Gleason score 7 on biopsy for men being considered for active surveillance [5]. For the appropriate patient, depending on age, comorbidity, extent of cancer, MRI findings, patient desire, etc., could be a candidate for active surveillance with Gleason score 3 + 4 = 7 if the pattern 4 is limited. Currently, this information is not transparent in most pathology reports.
A new grading system, first proposed in BJUI by this author, and verified in a large multi-institutional study, resulted in a simplified five-grade group system that more accurately reflects the biology of prostate cancer than the pre-2005 grading system [3, 6]. Men with Gleason score 6 cancers need to be reassured that their cancer is the lowest grade that is currently assigned, despite Gleason scores ranging from 2 to 10. In addition, I have talked to some patients with Gleason score 3 + 4 = 7 who think that they are going to die in the near future because their score of 7 was closer to highest grade of 10 than the lowest grade of 2. With the new grading system, patients can be reassured that they have a Grade group 1 (3 + 3 = 6) out of 5, which is the lowest grade, or a Grade group 2 (Gleason score 3 + 4 = 7) out of 5, which is still a relatively low grade.
Video: Gleason Grading in the Spotlight
The impact of the 2005 International Society of Urological Pathology consensus guidelines on Gleason grading – a matched pair analysis
Objectives
To investigate whether the International Society of Urological Pathology (ISUP) 2005 revision of the Gleason grading system has influenced the risk of biochemical recurrence (BCR) after radical prostatectomy (RP), as the new guideline implies that some prostate cancers previously graded as Gleason score 6 (3 + 3) are now considered as 7 (3 + 4).
Patients and methods
A matched-pair analysis was conducted. In all, 215 patients with Gleason score 6 or 7 (3 + 4) prostate cancer on biopsy who underwent RP before 31 December 2005 (pre-ISUP group), were matched 1:1 by biopsy Gleason score, clinical tumour category, PSA level, and margin status to patients undergoing RP between 1 January 2008 and 31 December 2011 (post-ISUP group). Patients were followed until BCR defined as a PSA level of ≥0.2 ng/mL. Risk of BCR was analysed in a competing-risk model.
Results
The median follow-up was 9.5 years in the pre-ISUP group and 4.8 years in the post-ISUP group. The 5-year cumulative incidences of BCR were 34.0% and 13.9% in the pre-ISUP and post-ISUP groups, respectively (P < 0.001). The difference in cumulative incidence applied to both patients with Gleason score 6 (P < 0.001) and 7 (3 + 4) (P = 0.004). There was no difference in the 5-year cumulative incidence of BCR between patients with pre-ISUP Gleason score 6 and post-ISUP Gleason score 7 (3 + 4) (P = 0.34). In a multiple Cox-proportional hazard regression model, ISUP 2005 grading was a strong prognostic factor for BCR within 5 years of RP (hazard ratio 0.34; 95% confidence interval 0.22–0.54; P < 0.001).
Conclusion
The revision of the Gleason grading system has reduced the risk of BCR after RP in patients with biopsy Gleason score 6 and 7 (3 + 4). This may have consequences when comparing outcomes across studies and historical periods and may affect future treatment recommendations.
West Coast Urology : Highlights from the AUA 2016 in San Diego… Part 1
By Ben Challacombe (@benchallacombe) and Jonathan Makanjuola (@jonmakurology)
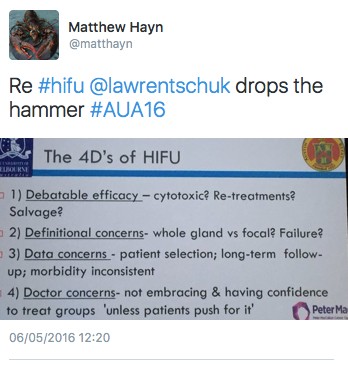
The 2016 AUA returned to the beautiful city of San Diego set on the shores of the Pacific in an excellent conference centre located in the centre of the town adjacent to the Gaslamp district. For a change the wifi was excellent and allowed enhanced levels of social media interaction and urological discussion. Opening these interactions were 2 key sessions which provoked much debate. Firstly the announcement that after over 10 years of trying the FDA has approved HIFU treatment although it seemed to get there through a slightly “de novo” pathway. Apparently the FDA approved it as an ablation tools but not for prostate cancer.
Although not directly approved for use in prostate cancer, that is exactly what it is going to be used for. A packed house saw a debate with evidence from both sides. Dr Nathan Lawrentschuk promoted the 4 Ds of HIFU. His key point was that 56/101 had a post treatment biopsy of which 51 where biopsy positive!
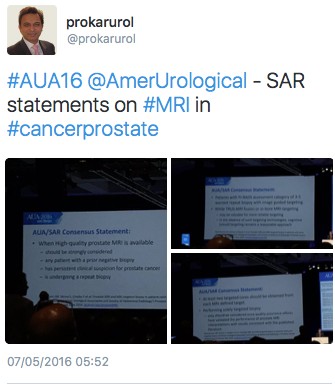
The second big session focussed on the AUA/SAR consensus statement document on prostate cancer diagnostics. This recommended a “High Quality” MRI should be strongly considered if patient has a rising PSA with a previous negative biopsy, has persistent clinical suspicion for prostate cancer or is undergoing a repeat biopsy. There was no mention of MRI for all at the pre-biopsy stage which many had hoped for and only 2 lines on trans-perineal biopsy as an option. This is of course related to health resources and the outpatient office-based nature of most USA urologists.
A welcome innovation was the Crossfire Sessions which pitted 2 well known advocates of one treatment against 2 with the opposite views. It was hardly debating of the Oxbridge variety but none the less did provoke some useful discussions. Topics included radical prostatectomy vs radiotherapy, endoscopic vs nephro-ureterectomy management of upper tract TCC, and enucleation at partial nephrectomy vs formal resection. Standing room only at the back of the halls but no real audience interaction or voting which was a shame.
The session which really woke everyone up was Rene Sotalo’s wonderful complication horror show. Bleeding, bleeding and more bleeding in a variety of ways. How would you handle this he asked? Pray I thought! But this and similar sessions clearly show the benefits of recording all cases and reviewing these DVDs if something goes wrong. The cause of some complications were only identified by review of the intra-operative tapes. Some clinical titbits learn’t included using only a horizontal incision for the camera port at RARP to reduce hernias and turning off pneumocompression stockings if there is a major venous injury to prevent excessive venous bleeding.
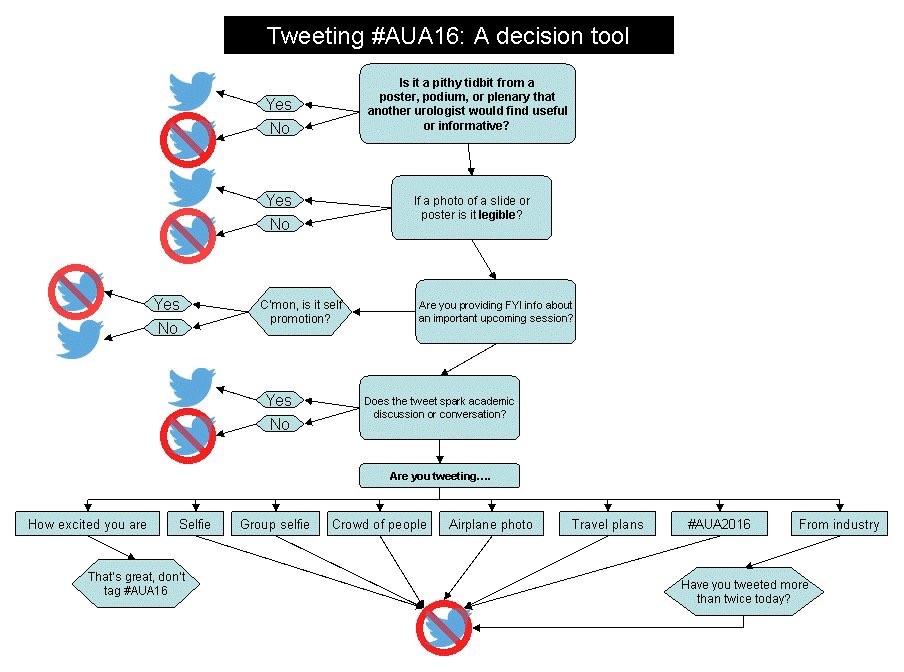
From a SoME perspective there was both good and bad. One poster showed that 40% of graduating US residents had publicly accessible unprofessional content on social media. Food for thought at the consultant interview no doubt, but on the other side SoMe ranks third in the acquisition of urological knowledge (and climbing…). One hack produced this tweeting guideline for all to reflect on.
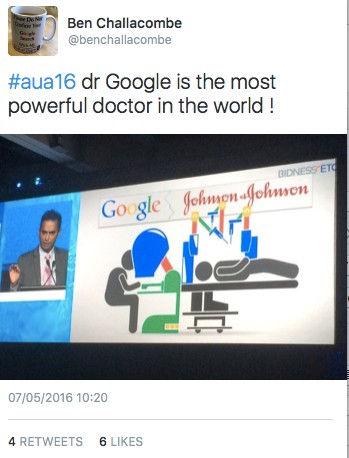
Prof Prokar Dasgupta had the honour of presenting the widely anticipated session on emerging robotic technology . At last there appears to be some real competition to Intuitive’s dominance on the way. There are at least 3 credible robotic systems on the way. He finished with an intriguing slide on Dr Google being the most powerful doctor in the world!
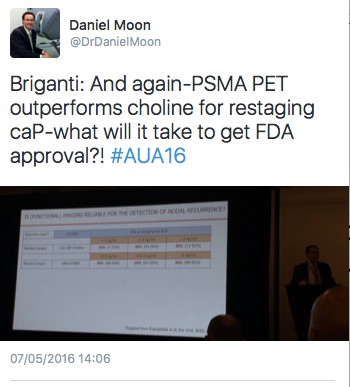
Despite Europe and Asia moving towards the use of PMSA PET , the USA is not moving in this direction due to reimbursement issues if the PMSA molecule.
There was a lot of interest in a packed auditorium to see live surgery for a single use disposable fURS “Lithovue” with some reporting superior vision , optics and deflection.
There were some sceptics amongst the stone community with the environmental impact and cost effectiveness a concern.
With the popular Gaslamp district a stones throw away many delegates went after the conference for a meal and drinks. The local baseball team San Diego Padres was a popular destination with may watching baseball for the 1st time whist others had gone for a run along the harbour and even caught a sighting of some seals!
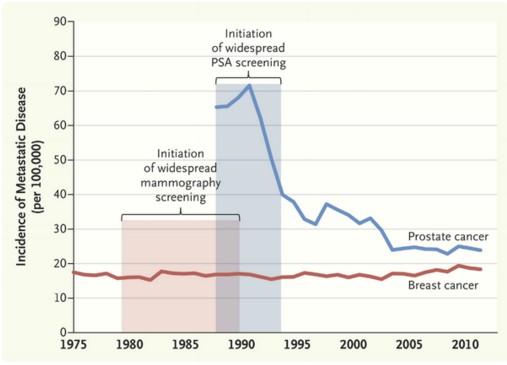
Does presentation with metastatic prostate cancer matter?
 November saw the return of the International Urology Journal Club #urojc on Twitter. The annual meetings of the World Congress for Endourology (#WCE2015) and Société Internationale D’Urologie (#SIU15) led to an October break for #urojc. This month’s discussion was based around a recent editorial in the New England Journal of Medicine by Welch et al on the effects of screening on the incidences of metastatic-at-diagnosis prostate and breast cancers. In the three days prior to the start of the discussion the editorial and it’s now well-known graph had been trending amongst medical Twitter users.
November saw the return of the International Urology Journal Club #urojc on Twitter. The annual meetings of the World Congress for Endourology (#WCE2015) and Société Internationale D’Urologie (#SIU15) led to an October break for #urojc. This month’s discussion was based around a recent editorial in the New England Journal of Medicine by Welch et al on the effects of screening on the incidences of metastatic-at-diagnosis prostate and breast cancers. In the three days prior to the start of the discussion the editorial and it’s now well-known graph had been trending amongst medical Twitter users.
The issue of PSA screening for prostate cancer has been a topic of debate amongst urologists for a number of years. PSA and DRE are first line for early detection of prostate cancer. Supporters of PSA screening argue that it leads to a significant fall in prostate cancer specific mortality. Many others believe there is insufficient evidence to support universal PSA screening given the risks of prostate biopsy and potential overtreatment of low risk prostate cancer.
The editorial presented data showing a significant fall in the number of patients first presenting with metastatic prostate cancer (advanced stage incidence) following the introduction of universal screening. However no effect was shown on similar data for breast cancer. Variations in disease dynamics were suggested to play a role.
The conversation started on Sunday 1st November at 20:00 (GMT), marking the beginning of the fourth year of #urojc. The first questions centred around the reasons behind the trends seen in the graph. Being a urology journal club the conversation was based almost exclusively on the prostate cancer aspect of the editorial.
One suggestion for the discrepancy between the two cancers is that PSA is a better detector of metastatic disease, whilst mammography can only detect localised disease.
Based on incidence of metastatic prostate cancer, the article makes a convincing statement in support of universal PSA screening. However, a successful screening programme should result in a reduction in the incidence of advanced cancers, decreased advanced-stage incidence and reduced mortality. Leading to the question of whether looking solely at advanced-stage incidence is useful.
The importance of responsible treatment and active surveillance was mentioned early on.
One of the most important questions of the discussion: What impact and relevance does the image have? Views were polarised. Some contributors were cautious about drawing conclusions from the graph whilst others were satisfied that it justified PSA screening.
The article drew comparison between Halsted’s and Fisher’s descriptions of cancer progression. Halsted suggested cancer originates from a single site and spreads, whereas Fisher’s paradigm proposed that breast cancer is a systemic disease by the time it is detectable.
The United States Preventive Services Task Force (USPSTF) has recommended against universal screening of prostate cancer, suggesting the risks of testing outweighed the benefits. However, many believe this to be based on outdated evidence.
The Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial results showed a 12% higher incidence of prostate in the screening arm versus control, with no difference in mortality. Yet, the European Randomized Study of Screening for Prostate Cancer (ERSPC) has shown screening to result in a 1.6 fold increase in prostate cancer with a 21% reduction in mortality.
The debate briefly discussed the morbidity and cost of metastatic disease.
The editorial certainly raised a number of interesting points. It seems the topic of universal PSA screening will continue to be debated. There is a significant benefit to screening in the prevention of metastatic prostate cancer. Whether this is due to differing disease dynamics or PSA being a better screening tool than mammography is as yet unclear.
One point we can all agree on is that increasing utilisation of active surveillance with timely biopsies is important in preventing overtreatment of low risk disease and identifying those at risk of disease progression for curative treatment.
Anthony Noah Urology Speciality Trainee, West Midlands, UK
Twitter: @antnoah
Abandoning PSA screening: What is an acceptable price to pay?
 The PSA screening debate continues to rage with conflicting advice from various bodies as to appropriate guidelines for men considering prostate cancer screening. In Australia the Urological Society of Australia and New Zealand (USANZ) has supported offering screening to men aged 55-69 [Urological Society of Australia and New Zealand Position Statement on PSA testing 2009], as has the Royal Australasian College of Pathologists [Royal College of Pathologists Australia Position Statement on PSA testing 2014], however the guidelines for General Practitioners is yet to endorse this approach. A consensus group gathered by the Cancer Council of Australia, including Urologists, Oncologists, Epidemiologists and consumer advocates have recently put together proposals being considered by the NHMRC that recommend screening in men of an appropriate age with >7 year life expectancy, as long as active surveillance is offered to those diagnosed with low risk disease [Cancer Council Australia: Draft Clinical Practice Guideline PSA Testing and Early Management of Test-Detected Prostate Cancer]. The US Preventative Service Task Force Grade D recommendation against screening has been well documented, yet widely criticized for failing to include Urologists in its deliberations – the very specialists tasked with evaluating and treating localized prostate cancer.
The PSA screening debate continues to rage with conflicting advice from various bodies as to appropriate guidelines for men considering prostate cancer screening. In Australia the Urological Society of Australia and New Zealand (USANZ) has supported offering screening to men aged 55-69 [Urological Society of Australia and New Zealand Position Statement on PSA testing 2009], as has the Royal Australasian College of Pathologists [Royal College of Pathologists Australia Position Statement on PSA testing 2014], however the guidelines for General Practitioners is yet to endorse this approach. A consensus group gathered by the Cancer Council of Australia, including Urologists, Oncologists, Epidemiologists and consumer advocates have recently put together proposals being considered by the NHMRC that recommend screening in men of an appropriate age with >7 year life expectancy, as long as active surveillance is offered to those diagnosed with low risk disease [Cancer Council Australia: Draft Clinical Practice Guideline PSA Testing and Early Management of Test-Detected Prostate Cancer]. The US Preventative Service Task Force Grade D recommendation against screening has been well documented, yet widely criticized for failing to include Urologists in its deliberations – the very specialists tasked with evaluating and treating localized prostate cancer.
Screening trials have reported conflicting results [Schroder et al, Pinsky et al], however with longer follow-up it becomes easier to demonstrate a survival advantage in men who are screened, and this does not even directly take into account the reduction in morbidity from advanced disease in populations as a result of early detection.
The issue at hand seems inherently very simple – that mass PSA screening will inevitably lead to overdiagnosis and, if a conservative approach is not adopted in low-risk disease or men with significant co-morbidities, overtreatment. Since PSA testing was introduced, the natural history of prostate cancer has become better understood [Albertsen], along with the understanding that many men with prostate cancer harbor “clinically insignificant” disease. Urologists have recognized this internationally and developed active surveillance protocols in response [Kates et al, Klotz]. Here in Australia the Victorian prostate cancer registry now confirms a significant number of men with low-risk disease being managed conservatively [Evans].
In the meantime, however, the pendulum is swinging the other way, and on the back of the USPSTF recommendations we are now seeing evidence of a drop in PSA screening. Confusing the debate is the extrapolation of negative studies to men of an entirely different population (e.g. using the Prostate Cancer Intervention vs Observation Trial [PIVOT], which comprised an average age of 67 to conclude that men in their 50s will not benefit from screening), poor design of the reported screening trials (e.g. the PLCO trial, which formed the backbone of USPSTF recommendations but due to compliance/contamination compared a population of 52% screened vs 85% screened), and the accusations of vested interests, particularly when Urologists take a pro-screening position (just read comment section on BJUI 2013 report of “Melbourne consensus statement on prostate cancer testing”)
What is the end result at a population level? In Victoria, Cancer Council data confirm a drop in prostate cancer screening and diagnosis [FIGURE]. There is no reason to believe that true prostate cancer incidence has suddenly declined, and we can conclude therefore that the negative publicity surrounding PSA screening is having an impact and less men are undertaking screening and diagnosis; a reversal of the jump in incidence that occurred when PSA testing was first introduced. Is this a bad thing though? Could this just be that we are finally reducing the diagnosis of clinically irrelevant cancers that are the bane of a PSA screening programme?
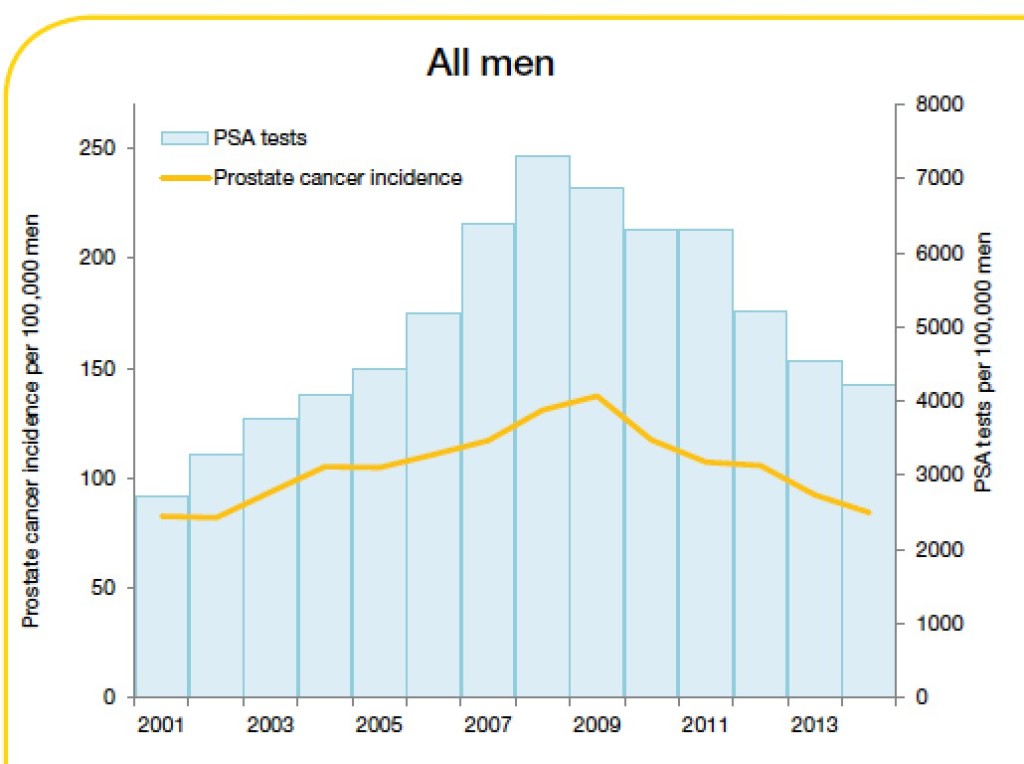
Trends in prostate cancer incidence and PSA testing rates, 2001-2014
Source: Cancer in Victoria: Statistics and Trends 2014. Cancer Council Victoria
My disclosure is that as a Urologist with a subspecialty practice in prostate cancer management, I deal at a personal level with patients, rather than population statistics, and in the last few months alone, multiple patients have highlighted for me the sacrifice we must admit to making if we are to abandon or even discourage PSA testing. A few specific cases are worth sharing as scenarios that GPs could consider including in the risk/benefit discussion required before ordering a PSA test.
Case 1:
64-year-old, well man with no relevant past/family history was referred with a rising PSA from 3.9μg/L in 2010 to 6.6μg/L in 2011. No abnormality was found on rectal examination and a biopsy was advised but refused given contemporary publicity in the lay press outlining the risk of biopsy and harms of overdiagnosis/overtreatment. Over the next 5 years the patient undertook various natural remedies and in 2014 when the PSA was 13.3μg/L, an MRI was performed that demonstrated a PIRADS 4 lesion. It was only until 2015 when the PSA had reached 21.9μg/L that a biopsy demonstrated a significant volume of Gleason 9 adenocarcinoma, with pelvic lymphadenopathy on staging.
Case 2:
A 57-year-old man requested PSA screening in 2013; however, he was advised by his local doctor that this was unnecessary based on current guidelines. In 2015 the patient’s brother was diagnosed elsewhere with prostate cancer and underwent radical prostatectomy. The patient then demanded a PSA, which was performed and found to be 40μg/L. Rectal examination revealed a firm, clinical stage T3 malignancy and biopsy demonstrated extensive Gleason 4+4 prostate cancer.
Case 3:
A 51-year-old man was found in 2010 to have a mildly elevated screening PSA of 4.5μg/L. Despite repeated recalls from the GP to have this repeated and further investigated the patient refused until in 2015 he presented with obstructive voiding symptoms and was found on examination to have a diffusely firm, clinical stage T3 malignant prostate. Repeat PSA was 39μg/L and subsequent investigation confirmed extensive Gleason 9 prostate cancer with positive pelvic lymph nodes.
For these men curative treatment is probably no longer an option. Whilst a small anecdotal group, these are real men seen at a community level who demonstrate the power of PSA screening to identify aggressive, clinically significant disease, at an early, curable stage. This is the coalface that General Practitioners and Urologists work at. When the USPSTF ratifies the Grade D recommendations on the basis of flawed and often misinterpreted trials in the absence of specialists who treat such patients, when Epidemiologists and well-meaning Oncologists who never see or evaluate localized prostate cancer lobby against the harms of overdiagnosis and overtreatment, they are condemning these men, and many others, to suffer and die from a preventable disease.
This risk of increased advanced cancer in a non-screened population has already been foreseen and reported [Scosyrev]. How many such men is it acceptable to sacrifice in the name of preventing overdiagnosis and overtreatment?
Rather than the knee-jerk response to abandon PSA testing, the answer, which is increasingly accepted by Urologists, is clearly to unlink prostate cancer diagnosis from treatment. It is to improve diagnostics as we are seeing with development of multiparametric MRI and molecular/genetic markers to make screening and treatment selection smarter. I fear that if this is not more widely accepted and the current situation continues, it is helpful that so much research is being conducted in the management of men with high-risk, oligometastatic and advanced disease, because it will be more and more of these cancers that we will be treating.
Dr Daniel Moon is Director of Robotic Surgery at the Epworth Healthcare, and a Urologist at the Peter MacCallum Cancer Institute, Melbourne
@drdanielmoon
Controversies in management of high-risk prostate and bladder cancer
 Recently, there has been substantial progress in our understanding of many key issues in urological oncology, which is the focus of this month’s BJUI. One of the most substantial paradigm shifts over the past few years has been the increasing use of radical prostatectomy (RP) for high-risk prostate cancer and increasing use of active surveillance for low-risk disease [1,2].
Recently, there has been substantial progress in our understanding of many key issues in urological oncology, which is the focus of this month’s BJUI. One of the most substantial paradigm shifts over the past few years has been the increasing use of radical prostatectomy (RP) for high-risk prostate cancer and increasing use of active surveillance for low-risk disease [1,2]. References
Article of the Month: Indications for Intervention During Active Surveillance of Prostate Cancer
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Max Kates discussing his paper.
If you only have time to read one article this week, it should be this one.
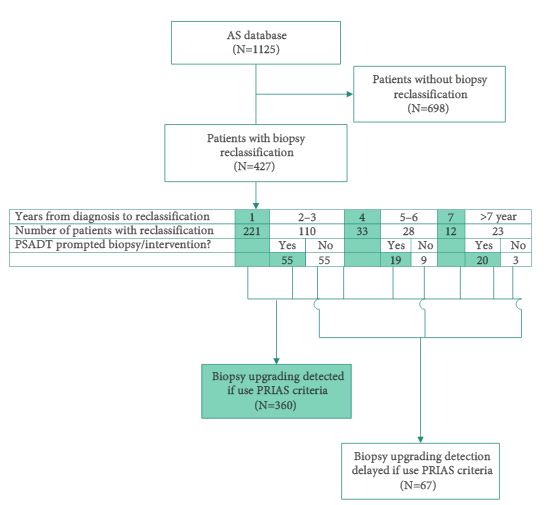
Indications for Intervention During Active Surveillance of Prostate Cancer: A Comparison of the Johns Hopkins and PRIAS Protocols
OBJECTIVE
To analyse how patients enrolled in our biopsy based surveillance programme would fare under the Prostate Cancer Research International Active Surveillance (PRIAS) protocol, which uses PSA kinetics.
PATIENTS AND METHODS
Since 1995, 1125 men with very-low-risk prostate cancer have enrolled in the AS programme at the Johns Hopkins Hospital (JHH), which is based on monitoring with annual biopsy. The PRIAS protocol uses a combination of periodic biopsies (in years 1, 4, and 7) and prostate-specific antigen doubling time (PSADT) to trigger intervention. Patients enrolled in the JHH AS programme were retrospectively reviewed to evaluate how the use of the PRIAS protocol would alter the timing and use of curative intervention.
RESULTS
Over a median of 2.1 years of follow up, 38% of men in the JHH AS programme had biopsy reclassification. Of those, 62% were detected at biopsy intervals corresponding to the PRIAS criteria, while 16% were detected between scheduled PRIAS biopsies, resulting in a median delay in detection of 1.9 years. Of the 202 men with >5 years of follow-up, 11% in the JHH programme were found to have biopsy reclassification after it would have been identified in the PRIAS protocol, resulting in a median delay of 4.7 years to reclassification. In all, 12% of patients who would have undergone immediate intervention under PRIAS due to abnormal PSA kinetics would never have undergone reclassification on the JHH protocol and thus would not have undergone definitive intervention.
CONCLUSIONS
There are clear differences between PSA kinetics-based AS programmes and biopsy based programmes. Further studies should address whether and how the differences in timing of intervention impact subsequent disease progression and prostate cancer mortality.