Video: Penile vibratory stimulation after radical prostatectomy
Penile vibratory stimulation in the recovery of urinary continence and erectile function after nerve-sparing radical prostatectomy: a randomized, controlled trial
Mikkel Fode*, Michael Borre†, Dana A. Ohl‡, Jonas Lichtbach§ and Jens Sønksen*
*Department of Urology, Herlev University Hospital, Herlev, †Department of Urology, Aarhus University Hospital, Aarhus, Denmark, ‡Department of Urology, University of Michigan, Ann Arbor, MI, USA, and §Department of Physiotherapy, Herlev University Hospital, Herlev, Denmark
OBJECTIVE
• To examine the effect of penile vibratory stimulation (PVS) in the preservation and restoration of erectile function and urinary continence in conjunction with nerve-sparing radical prostatectomy (RP).
PATIENTS AND METHODS
• The present study was conducted between July 2010 and March 2013 as a randomized prospective trial at two university hospitals. Eligible participants were continent men with an International Index of Erectile Function-5 (IIEF-5) score of at least 18, scheduled to undergo nerve-sparing RP.
• Patients were randomized to a PVS group or a control group. Patients in the PVS group were instructed in using a PVS device (FERTI CARE® vibrator).
• Stimulation was performed at the frenulum once daily by the patients in their own homes for at least 1 week before surgery. After catheter removal, daily PVS was re-initiated for a period of 6 weeks.
• Participants were evaluated at 3, 6 and 12 months after surgery with the IIEF-5 questionnaire and questions regarding urinary bother. Patients using up to one pad daily for security reasons only were considered continent. The study was registered at https://clinicaltrials.gov/ (NCT01067261).
RESULTS
• Data from 68 patients were available for analyses (30 patients randomized to PVS and 38 patients randomized to the control group).
• The IIEF-5 score was highest in the PVS group at all time points after surgery with a median score of 18 vs 7.5 in the control group at 12 months (P = 0.09), but the difference only reached borderline significance.
• At 12 months, 16/30 (53%) patients in the PVS group had reached an IIEF-5 score of at least 18, while this was the case for 12/38 (32%) patients in the control group (P = 0.07).
• There were no significant differences in the proportions of continent patients between groups at 3, 6 or 12 months. At 12 months 90% of the PVS patients were continent, while 94.7% of the control patients were continent (P = 0.46).
CONCLUSION
• The present study did not document a significant effect of PVS. However, the method proved to be acceptable for most patients and there was a trend towards better erectile function with PVS. More studies are needed to explore this possible effect further.


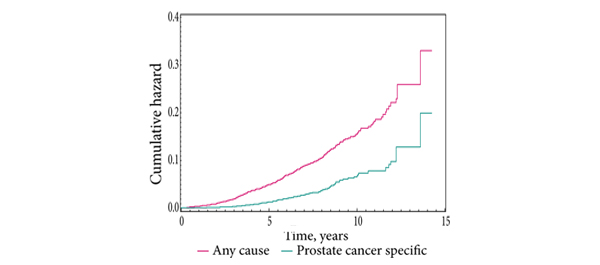


 In this week’s edition of the NEJM, Anna Bill-Axelson and the Scandinavian Prostate Cancer Group Study Number 4 (SPCG-4) investigators have
In this week’s edition of the NEJM, Anna Bill-Axelson and the Scandinavian Prostate Cancer Group Study Number 4 (SPCG-4) investigators have