Editorial: Does knowing the risk of relapse in localized renal cell carcinoma matter?
Shah et al. [1] report a retrospective analysis from the Mayo Clinic investigating the prognostic significance of different patterns of pathological T3a clear‐cell RCC in patients who underwent radical nephrectomy for localized disease. There was no difference in disease progression, cancer‐specific mortality or all‐cause mortality when comparing isolated perinephric fat invasion vs isolated renal sinus fat invasion vs isolated renal vein invasion. Multiple sites of extra‐renal extension compared with one site, however, was independently associated with an increased risk of disease progression (hazard ratio [HR] 1.31, P = 0.02), death from RCC (HR 1.64, P < 0.001) and all‐cause mortality (HR 1.32, P = 0.008) when adjusting for multiple key variables including age, tumour size, grade, presence of coagulative tumour necrosis and sarcomatoid differentiation. The authors incorporated multiple sites of extra‐renal extension vs one site into three RCC prognostic models: SSIGN score, UISS and MSKCC nomogram. After controlling for these three predictive tools independently, multiple sites of extra‐renal disease predicted progression, death from RCC and all‐cause death. These data suggest that risk stratification for pT3aN0MO clear‐cell RCC is improved by differentiating multiple vs one site of extra‐renal extension.
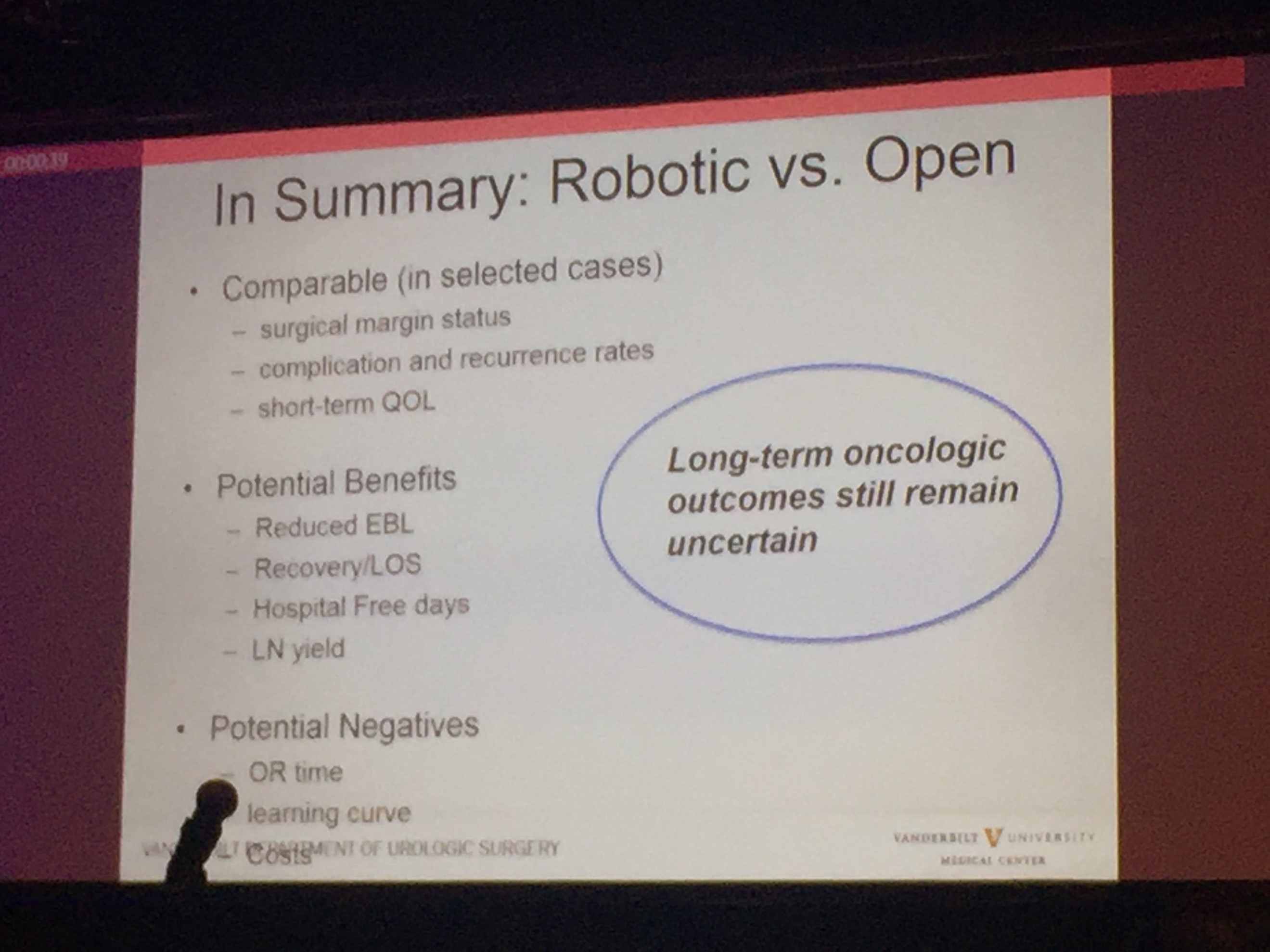
Does an improved ability to predict recurrence and mortality increase the likelihood of cure in high‐risk localized RCC patients in 2018? Unfortunately, the answer is no. Ideally, prognostic models would identify patients at sufficient risk to consider adjuvant therapy, which would increase cure rates by eradicating micro‐metastatic disease with an acceptable toxicity. Regrettably, in RCC management there are no well‐established post‐surgical therapies that improve cure rates. The deficiency of established adjuvant therapies is not attributable to a lack of investigative trials. In the era before vascular endothelial growth factor receptor (VEGFR) targeting, adjuvant vaccines, immunotherapies and other systemic therapies failed to demonstrate improved recurrence‐free (RFS) or overall survival (OS) [2]. The efficacy of VEGFR‐targeted therapies in the metastatic setting re‐energized the hope for adjuvant therapy in patients with high‐risk localized RCC after surgical resection in the past two decades. The results to date have been disappointing. To date, three trials (ASSURE, PROTECT and S‐TRAC) have been completed, comparing oral VEGFR tyrosine kinase inhibitors with placebo in high‐risk localized clear‐cell RCC, with disease‐free survival (DFS) as the primary endpoint [3,4,5]. ASSURE and PROTECT showed no difference in RFS or OS [3,4,5]. S‐TRACT demonstrated an improvement in DFS but not in OS [4]. A pooled analysis of these three trials also failed to demonstrate improved DFS or OS with adjuvant VEGFR‐targeted therapy [6]. Significant side effects with discontinuation of adjuvant therapy occurred in 28–45% of patients as a result of drug‐related toxicity [6]. Trials investigating immune checkpoint inhibitors have yet to be published and, with the established efficacy of these drugs in the metastatic setting, hope still remains for adjuvant therapy in resected high‐risk localized RCC.
If the current literature does not support adjuvant therapy for resected high‐risk RCC, does knowing the risk of relapse alter surveillance? National Comprehensive Cancer Network guidelines for resected stage III RCC recommend chest and abdominal imaging within 3–6 months, along with subsequent chest and abdominal imaging every 3–6 months for 3 years, and then annually up to 5 years. Although the ideal schedule for surveillance imaging is unknown, further characterizing of the risk of relapse in high‐risk localized RCC would not be likely to affect this schedule significantly.
Although knowing the risk of relapse in high‐risk localized RCC does not help management in 2018, there is still a value to enhancing our prognostic tools. For one, our prognostic tools help clinicians counsel patients appropriately about their risk of recurrence. In addition, enhanced prognostic tools will assist in selecting appropriate patients with high‐risk localized RCC for future clinical trials of adjuvant therapy and also help us understand the results when comparing cohorts within and between trials.
References
- Shah PH, Lyon TD, Lohse CM. Prognostic evaluation of perinephric fat, renal sinus fat, and renal vein invasion for patients with pathologic stage T3a clear cell renal cell carcinoma. BJU Int 2019; 123: 270–6
- Scherr AJO, Lima JPSN, Sasse EC et al. Adjuvant therapy for locally advanced renal cell cancer: a systematic review with meta‐analysis. BMC Cancer 2011; 11: 115–21
- Haas N, Manola J, Uzzo R et al. Adjuvant sunitinib or sorafenib for high‐risk, non‐metastatic renal‐cell carcinoma (ECOG‐ACRIN E2805): a double‐blind, placebo‐controlled, randomised, phase 3 trial. Lancet 2016; 387: 2008–16
- Ravaud A, Motzer RJ, Pandha HS et al. Adjuvant sunitinib in high‐ risk renal‐cell carcinoma after nephrectomy. N Engl J Med 2016; 375: 2246–54
- Motzer RJ, Haas NB, Donskov F et al. Randomized phase III trial of adjuvant pazopanib versus placebo after nephrectomy in patients with localized or locally advanced renal cell carcinoma. J Clin Oncol 2017; 35: 3916–23
- Sun M, Marconi L, Eisen T et al. Adjuvant vascular endothelial growth factore‐targeted therapy in renal cell carcinoma. Eur Urol 2018; 74: 611–20