Article of the Week: Prospective randomised non-inferiority trial of PD placement vs ND placement after RARP
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this month, it should be this one.
Prospective randomised non-inferiority trial of pelvic drain placement vs no pelvic drain placement after robot-assisted radical prostatectomy
Abstract
Objective
To determine if eliminating the prophylactic placement of a pelvic drain (PD) after robot-assisted radical prostatectomy (RARP) affects the incidence of early (90-day) postoperative adverse events.
Patients and Methods
In this parallel-group, blinded, non-inferiority trial, we randomised patients planning to undergo RARP to one of two arms: no drain placement (ND) or PD placement. Patients with demonstrable intraoperative leakage upon bladder irrigation were excluded. Randomisation sequence was determined a priori using a computer algorithm, and included a stratified design with respect to low vs intermediate/high D’Amico risk classifications. Surgeons remained blinded to the randomisation arm until final eligibility was verified at the end of the RARP. The primary endpoint was overall incidence of 90-day complications which, based on our standard treatment using PD retrospectively, was estimated at 13%. The non-inferiority margin was set at 10%, and the planned sample size was 312. An interim analysis was planned and conducted when one-third of the planned accrual and follow-up was completed, to rule out futility if the delta margin was in excess of 0.1389.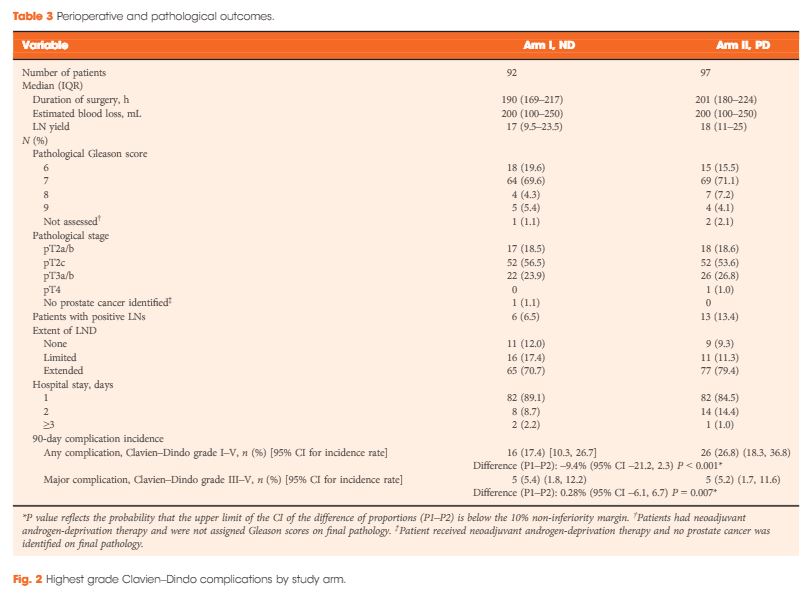
Results
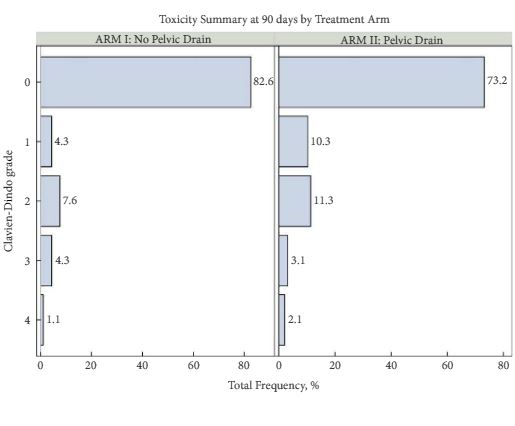
From 2012 to 2016, 189 patients were accrued to the study, with 92 patients allocated to the ND group and 97 to the PD group. Due to lower than expected accrual rates, accrual to the study was halted by regulatory entities, and we did not reach the intended accrual goal. The ND and PD groups were comparable for median PSA level (6.2 vs 5.8 ng/mL, P = 0.5), clinical stage (P = 0.8), D’Amico risk classification (P = 0.4), median lymph nodes dissected (17 vs 18, P = 0.2), and proportion of patients receiving an extended pelvic lymph node dissection (70.7% vs 79.4%, P = 0.3). Incidence of 90-day overall and major (Clavien–Dindo grade >III) complications in the ND group (17.4% and 5.4%, respectively) was not inferior to the PD group (26.8% and 5.2%, respectively; P < 0.001 and P = 0.007 for difference of proportions <10%, respectively). Symptomatic lymphocoele rates (2.2% in the ND group, 4.1% in the PD group) were comparable between the two arms (P = 0.7).
Conclusions
Incidence of adverse events in the ND group was not inferior to the group who received a PD. In properly selected patients, PD placement after RARP can be safely withheld without significant additional morbidity.