Société Internationale d’Urologie : Buenos Aires 2016
Hola como estas? The 36th SIU congress was held in Buenos Aires, Argentina 20-24th October. Their motto: ‘we bring urologists together’ was certainly fulfilled as reflected by the warm atmosphere and international mix of speakers and attendees. The scientific programme included plenary sessions, debates, hands on instructional courses, trainee Q&A sessions and symposiums.
The location and facilities at the Hilton were first class. A large exhibition hall allowed for interaction with industry. The use of the pool bar hosted by the SIU innovators group was a particular highlight.
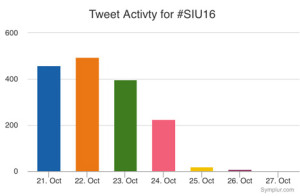
The conference app was easy to use and the conference hashtag #SIU16 and a #selfie challenge were promoted. The selfie prize of a trip to SIU Portugal was won by Argentine resident Dr. Jose Nolazco with over 300 likes!
The conference kicked off with varied and interesting sessions on a range of urology, which included sub-section meetings such as societies of the Middle East, Africa, Asia, and Argentina; plus the 2nd SIU nurses educational symposium. The most popular meeting (in numbers attending and discussions after) was the World Urological Oncology Federation Symposium (WUOF). A delegate from South Africa told me that he appreciated the summary of new research and highlighting the areas of change, especially in a field when advances can occur quickly, for example PMSA-PET which may be able to give more information on metastatic prostate cancer than MRI. Arnaud Villiers vs Robert Reiter debated the issue of focused vs radical therapy to an intermediate, solitary lesion in the prostate. Reiter argued NOT for focal therapy on the basis of the imperfections of the MRI.
The MRI-TRUS fusion course, hosted by SIU Innovators division and with MIMS from industry present, championed MRI as a primary diagnostic test to investigate prostate cancer. Boris Hadaslick quoted (PROMIS trial) that TRUS biopsy without MRI had a 50% chance of finding cancer: ‘like flipping a coin’. He emphasised that targeted plus systematic biopsy sampling was best practice and highlighted the fusion software systems can improve cancer diagnosis. However cognitive fusion can be as good.
Speakers enthusiastic about advances in urology described high costs that had to be justified to their healthcare system like PSMA-PET and immunotherapy for bladder cancer. Yet these costs would be impossible for other delegates to take back to their home countries. Indeed the most innovative speakers presented their cost-saving techniques in the ‘SANTU’ session; the opening remarks of ‘how can you drive a Ferrari if you don’t have paved roads?’ was particularly levelling. One speaker, Mohammed Lezrek, stood out as being particularly creative, which he says is as a result of necessity, he showed videos using rubber from syringes or saline bag ports to fix the bungs on his endoscopes in Morocco (https://m.youtube.com/user/lezrekmohamed). These are issues I wouldn’t even think to know how to fix, being fortunate enough to work in the NHS. Other speakers in the same session described using generic, mass produced Ureteric stents that were a fraction of the price, another described treating a condition common to him in Indonesia of penile dermatosclerosis caused by penile injections of oil obtained as easily as ‘getting a haircut’ with the low cost surgical technique of scrotal flap. There was also a symposium on Urology in the Developing World, which included the best-titled talk: ‘the hunt for the perfect penis’ given by Ms Rampersad. She is the only surgeon performing hypospadias repair in Trinidad and Tobago, at an incidence of 2.7 per 1000 live births and recommended that specialist surgery be performed by those who are keen and performing larger volumes.
The Endourology Society Symposium was a popular session with standing room only. There were lessons on the possibilities, but also the limitations of flexible ureteroscopy, including an impromptu debate on use of access sheath and a case of stone clearance in a patient with HSK. A Canadian audience member spoke of his difficulty in justifying the use of flexi URS to managers in view of longer operation time compared to PCNL due to OR pressure. Michael Grasso captivated the audience with his experience in using flexible URS for diagnosis and treating upper tract TCC. In his series this meant less nephrectomies, no dialysis and better palliation. He even does LA flexi URS in selected patients! An important message on the dangers of IntraRenal pressure was presented by Palle Osther, which can occur even at an irrigation height of 40cm. He highlighted that whilst papers are championing the use of Flexi URS in more complex cases this means more time in the renal pelvis with the added risk of complications. He quoted Hippocrates ‘do no harm’. Grasso and Olivier Traxer explained their methods of stringent use of irrigation via piston controlled syringe and limiting operation time to an hour.
 My personal highlight was the presentation of videos by Mr René Sotelo on ‘getting out of sticky situations’ (SIU innovators symposium). An expert panel described similar mistakes to the ones shown on the videos and added what they would do if faced with the problem, leading to a fruitful and rich discussion. He showed tachycardia inducing, faint provoking videos of bleeding from upper and lower tract minimally invasive surgery. Advice such as stay calm, phone a friend, increase the pneumo, ‘suture fast’ was useful and practical. One case showed a rectal perforation at cystectomy where the attending/junior had been asked to place a swab (on stick) into the vagina, but it became apparent once the swab was on show and the vagina was intact that the swab had been misplaced into the rectum, thus highlighting the need to know your anatomy! An amazing image of a Ureteric stent that had been accidentally placed in the atrium was shown; but we were told the next step should not be to call an endourologist!
My personal highlight was the presentation of videos by Mr René Sotelo on ‘getting out of sticky situations’ (SIU innovators symposium). An expert panel described similar mistakes to the ones shown on the videos and added what they would do if faced with the problem, leading to a fruitful and rich discussion. He showed tachycardia inducing, faint provoking videos of bleeding from upper and lower tract minimally invasive surgery. Advice such as stay calm, phone a friend, increase the pneumo, ‘suture fast’ was useful and practical. One case showed a rectal perforation at cystectomy where the attending/junior had been asked to place a swab (on stick) into the vagina, but it became apparent once the swab was on show and the vagina was intact that the swab had been misplaced into the rectum, thus highlighting the need to know your anatomy! An amazing image of a Ureteric stent that had been accidentally placed in the atrium was shown; but we were told the next step should not be to call an endourologist!
 In the opening ceremony we were welcomed by Argentine tango dancers, the Minister of Health: a qualified doctor with degree in public health, and some Argentine hospitality of wine and typical foods. Friendly and collegiate atmosphere is what the Secretary of the SIU promised us, and friendly banter was present during the day. The first Brexit joke came when Mr Chris Parker started to explain to one presenter of the World Oncology federation why the UK was not included in the observation of deterioration of prostate cancer outcomes during the 2008 world recession, to which the presenter replied that it was only European countries in the paper. There was a mix of cheers and boos from the audience. However UK prostate cancer research, such as the PROMIS trial and the Emberton team studies were frequently quoted, as well as other British papers, with high esteem as corner stones of cancer research and advancing patient care.
In the opening ceremony we were welcomed by Argentine tango dancers, the Minister of Health: a qualified doctor with degree in public health, and some Argentine hospitality of wine and typical foods. Friendly and collegiate atmosphere is what the Secretary of the SIU promised us, and friendly banter was present during the day. The first Brexit joke came when Mr Chris Parker started to explain to one presenter of the World Oncology federation why the UK was not included in the observation of deterioration of prostate cancer outcomes during the 2008 world recession, to which the presenter replied that it was only European countries in the paper. There was a mix of cheers and boos from the audience. However UK prostate cancer research, such as the PROMIS trial and the Emberton team studies were frequently quoted, as well as other British papers, with high esteem as corner stones of cancer research and advancing patient care.
Day 2 Friday
There was an early start for many who attended one of four optional instructional courses: each covered a different theme. I attended ‘management of priapism’ in view of its direct relevance to potential situations I may find myself in as an on call registrar. UCLH Consultants Asif Muneer and Guilio Garaffa hosted and gave clear information on acute management and surgical shunt techniques, plus imaging for more difficult cases, such as CT to exclude intra-abdominal cause of refractory priapism. The take home message was to consider early implantation of penile prosthesis if priapism lasts >72 hours. This was shown clearly on operative videos of prosthesis surgery at 3 weeks compared to 6 m; where the latter had penile fibrosis increasing surgical difficulty.
The first plenary session covered new advances in testicular cancer and another debate of focal therapy in intermediate prostate cancer. Scott Eggener presented a polished and compelling argument on why focal therapy could be the future, but Markus Graefen described his reluctance to accept it based on the research, limitations in MRI, and need for follow that is similar to active surveillance; but perhaps patient choice will drive us to make a conclusion. Fernando Secin described the low uptake of Active Surveillance within Argentina. This may be due to costs (both AS costs and costs lost by not operating) and lack of protocols; however, those clinicians who had undergone oncological training and worked in Academic centres were more likely to recommend AS.
Description of how Ebola affected our African colleagues and sadly mortality due to HSW highlights the breadth of education and world issues covered by the SIU congress. Winner of the SIU Astellas European Foundation Award, Dr John M Barry, described how five transplantation principles can be applied to urology. This included using life expectancy calculations, not age, in making decisions (he used his own Charlson comorbidity score to illustrate the point that it can be improperly used); he suggested using a quality of life grid and that practice guidelines, from numerous organisations use different grading systems thus he calls for unified, world scientific language.
I was invited to attend a ‘quick fire session for trainees’ where I met five experts and discussed career questions such as fellowships, choosing urology specialties and engaging with academia, which includes networking that we can practice during the conference. The experts were super friendly and one attendee was thrilled to meet Olivier Traxor who is his endourological hero.
Other sessions included the first session on ‘Professionalism in urology’ and included information on using Twitter and working with industry without compromising or influencing patient care by always practising evidence-based medicine. However, many researchers have ties to industry. Several tweets were shared during this session, for example:
How do we strike the right balance for industry support of medical education? @RenuEapen #SIU16 pic.twitter.com/MyVzxCLntA
— Henry Woo (@DrHWoo) October 21, 2016
Another session popular with trainees was ‘how to write a paper’ hosted by the World Journal of Urology.
Dan Wood from UCLH, UK chaired the session for congenital reconstruction, which included how to set up a service by Miss Claire Taylor; she emphasised the need to define the service you want to provide, decide which paediatric hospital you want to work with and having an excellent MDT and clinical specialist nurse, of which she is fortunate to have Winnie Nugent who works to bridge the gap between child and adult services.
The ‘Surgical Demo, session on Laparoscopy was well attended and the audience watched excellent videos from Karim Touijer on lap prostatectomy and Gonzalo Vitagliano on lap nephrectomy. The videos were clear and narration highlighted the relevant steps and anatomy. They emphasised the need to gain a mentor to reduce the learning curve and not attempt to set up a lap service solo. There was also an ‘encyclopaedic’ style Surgical Masters session of all types of prostate surgery for BPH that included surgical videos and tips/tricks.
Saturday
Many attended the sessions with a sore head on Saturday morning following the SIU Night party held at La Rural, a National Historic Landmark located in the Palermo district of Buenos Aires. It was inaugurated in the late 1800s in order to support and promote agricultural issues in Argentina. We were treated to typical foods: empanadas, freshly barbequed meats and sausages, breads and of course home grown wine. Entertainment was provided by Argentinian tango dancers and Argentine Gaucho dancers whose finale ended with Bolleadoras a dance that made hearts pound from the open male shirts, fast rhythm and the whirling ropes. Additionally, there was a photo booth for traditional Argentine dress, football snooker and a mechanical bull; luckily the only injury was an Australian trainee’s trousers.
The morning’s plenary session ‘Shifting sands – new technologies in stone disease’ covered a range of topics including retrograde intrarenal surgery by Mr Traxer. Mr Jorge Guitierrez highlighted the dangers of sepsis in stone disease; one key message included stopping stone surgery (including PCNL) when there was purulent urine. The panel agreed that 1-2cm stones fall in a grey area in the guidelines as to which treatment is the best. The majority of the panel favoured flexible ureteroscopy; but admitted that a patient’s ability to afford PCNL vs flexi URS and the surgeon’s skills and availability of equipment was what often governed practice rather than choice. Mariano Gonzalez described stone disease affecting pregnant women and the challenges of treating; interestingly he suggested that a low dose CT in the 2nd and 3rd trimester can be considered safe. Pradeep Rao informed us of the changing PCNL sizes and how the smaller ‘seeing needle scope’ at 4.8F enabled him to remove the stone in an infant less than one years old. Norberto Bernardo shared his experience with managing stones in complex patients, such as a case with severe scoliosis and another in a HSK. Mr Traxor made a plea that stents be used for the shortest time to reduce patient morbidity, i.e. as soon as they have been placed make a plan for ureteroscopy to enable stone treatment and removal.
The use of mesh for vaginal prolapse was debated by Nissrine Nakia (pro) and Paulo Palma (con). Palma highlighted the anatomy of the pelvic floor and the importance of identifying the level of deformity, which should then be used to select the right patients and select the correct procedure. The counter argument from Nakia started with a campaign slogan P.R.O.M.E.S.H in keeping with the ongoing US presidential debate. She stated that whilst the FDA did raise concerns regarding re-operation rates, there are now more modern meshes and are subjected to rigorous testing, plus experience has been gained regarding placement of mesh, post-mesh cystoscopy and use of oestrogen cream, which have all improved patient outcomes.
Meshes debate with Christian Cobreros, Nissrine Nakib & Hugo Davila @ #SIU16 pic.twitter.com/tur4uAEttG
— ALAPP (@ALAPPnews) October 22, 2016
Great pics of models showing pelvic floor anatomy -always a tricky concept! Mesh or not to mesh session #SIU16 pic.twitter.com/gO9jU0yQId
— Sophie Rintoul-Hoad (@urologytrainee) October 22, 2016
The European and Asian societies both presented in the plenary sessions. The EUA lecture, given by Arnulf Stenzl, described ongoing changes on how to improve TURBT, which included better training for juniors, including simulation, better visualisation (photo dynamic diagnosis) and the use of ‘bloc’ dissection with hybridknife to enable whole tumour removal in once piece, which can aid histological analysis.
Mr Foo from Singapore presented the UAA lecture on the subject of ‘holistic approach’ to care of BPH. Additionally that perhaps the Intro vesicular prostatic protrusion (IPP) tells us more about the likelihood of obstruction and when surgery would make the most difference.
Three parallel plenary sessions provided learning in the fields of spinal cord injury, paediatric urology and urological histology. The histology speakers had a tough job describing their field to us surgeons! The plenary session ‘SIU-ICD joint consultation on urological management of Spinal cord injury patients’ was well attended and covered the anatomy, surgical and non -surgical options, urodynamics and bladder emptying options. Speakers emphasised the need for Long-term follow-up, including upper tract imaging, blood tests (U&Es) and QOL questionnaires of which there are several. Each presenter clearly stated their recommendation and the level of evidence to support it. Tweets from this session included a commitment to reduce urine culture and treatment of UTI on asymptotic patients.
#SIU-ICUD on Uro Management of the #SCI Patient has been the result of a lot of work&collaboration. Congrats #SIU16 pic.twitter.com/ehIOWiOQuM
— Amanda Chung (@AmandaSJChung) October 22, 2016
‘Ageing and urology’ session complemented the holistic theme as an expert panel discussed optimisation of elderly patients and the difficult decision making process of offering surgery in patients with frailty, high risk GA and delirium and co-morbidities. One panellist said it was about making a judgement that if the patient will appreciate the change and it will add to their QOL then age is not a barrier to operating; however, teamwork with anaesthetists and geriatrics is key to optimisation.
Each day a ‘Surgical Demo’ session’ ran, Saturday’s was on stones which was, like many stone sessions, full; Perhaps highlighting the enthusiasm towards Endourology. Pictured is Mr Guitierrez describing correct ureteroscopic hand manoeuvres and his ‘painting’ technique to dust stones. Additionally Mr Lojanapiwat from Thailand presented his operative experience in subcostal access for upper pole stones.
Throughout the afternoon were moderated poster sessions; from reducing laparoscopic camera fogging to comparison of traditional vs western medicine. These accepted abstracts were presented by urologists who were at varying stages of their careers. Presentations reflected high standards of research and a culmination of hard work. After watching some of the poster presentations I joined the urethral reconstruction ‘surgical tips’ session, which drew the biggest audience. The presentations offered high-quality operative pictures and complimentary radiology pictures showing the complexity of some of these strictures. Daniela Andrich from UCLH presented their experience of post-traumatic strictures and emphasised that the mechanism of injury correlates to the stricture pattern. Furthermore that partial ureteric injuries are probably under reported as they heal with the catheter in situ, sited by the trauma/orthopaedic team.
Sunday
The sun shone brightly on the last day of the conference and whilst many In the city were enjoying their Sunday lie in or preparing for church, conference delegates made their way to the last four early morning instructional courses. I attended ‘surviving prostate cancer’ chaired by Prof Mundy, which covered the aftermath of treatment for prostate cancer: fistulae, strictures, incontinence. Interestingly as our colleagues in General Surgery change techniques it provides new challenges relating to recto-vesical fistulae. It was recommended that MRIs should include sagittal views to best define the fistula anatomy. Prof Mundy described the difficulty that radiotherapy creates by scarring the tissues, which makes these patients more at risk of post-operative complications. This means it’s imperative to properly assess people prior to radiotherapy, including a cystoscopy to assess the bladder (and if applicable the post-prostatectomy anastomosis). Then consent the patient thoroughly prior to radiotherapy so that they’re aware of the more difficult surgery they face, should it be required.
The plenary session started with four speakers describing the emerging role of immunotherapy and specifically in cancers of the prostate, bladder and kidney. The research presented gave optimism of improving treatments for these cancers and that trials are ongoing and concluding. Fred Saad described how access to tissue can try to develop precision medicine; mutations specific to that tumour and patient could be assessed and tested in the laboratory so that treatment can be targeted and avoid treatments that don’t work.
A fierce debate regarding the role of varicocele surgery in the era of assisted reproduction ended in favour of offering surgery. Robert Brannigan presenting the ‘yes’ argument argued that varicocelectomy needs to be synergistic to assisted contraception, especially if time is of the essence in relation to maternal age. He gave evidence that varicocelectomy improves sperm quality for assisted conception and sees changes 3 months post-surgery. Alex Pastusak said he’d rather be ‘successful than lucky’ and was in favour of assisted contraception as the evidence for varicocelectomy, even the meta-analysis papers, has limitations so casts doubt on validity of available studies.
Rene Sotelo presented his endoscopic techniques for fistula repair, which included lap or robotic surgery within the bladder to remove the tract, create a plane between the bladder and surrounding tissues, place omentum or fascia between and then close the defect. We quickly moved from advanced techniques to trying to establish the basic technique with the next speaker. Alain Houlgate described his experience of establishing an endourological teaching programme between France and Senegal, which cumulates in a diploma.
Abstract prize winner Henry Woo presented his work on the International journal club #urojc where each month newly published articles are sent out to twitter followers and discussion generated. Unsurprisingly he was congratulated via twitter:
@DrHWoo at Best Abstract Podium Pres : 38 countries involved in International Urol Journal Club #urojc ! #SIU16 pic.twitter.com/mDD6yp1nMS
— Amanda Chung (@AmandaSJChung) October 23, 2016
#Journal #club on #twitter for #urology. The future of learning? #urojc @SIU_urology #siu16 @sure_urology pic.twitter.com/qzy1uGrWKE
— Dr. M.S. Rahnama’i (@Dr_SRah) October 23, 2016
The last plenaries of the conference prior to further poster sessions included uroradiology, systemic cancer therapies and surgical demo on robotic cystectomy. The radiology session highlighted the advances in PSMA PET for prostate cancer recurrence but that TRUS still had a role.
PSMA & MRI #SIU16 @SIU_urology pic.twitter.com/4YcHqZ8AEi
— Luis Rico (@luisrico89) October 23, 2016
 River Plate Urological Meeting: representatives from the RSM – Urological section, UK, met with representatives from the Hospital Británicos in Rosario and Buenos Aires, Argentina and Montevideo, Uruguay. This is the first time these groups have met with the aim of collaboration and training. The day included presentations from the hospitals’ urology trainees, in English, on a range of topics and were marked as per the RSM marking criteria. The winning presentation was on ‘laparoscopic nephrectomy for living kidney donors’ and 2nd place for a presentation on ‘history of circumcision’. We had a tour of the hospital and were then welcomed into the British Embassy, to meet the Ambassador who is supportive of the relationships that are forming as a result of this meeting.
River Plate Urological Meeting: representatives from the RSM – Urological section, UK, met with representatives from the Hospital Británicos in Rosario and Buenos Aires, Argentina and Montevideo, Uruguay. This is the first time these groups have met with the aim of collaboration and training. The day included presentations from the hospitals’ urology trainees, in English, on a range of topics and were marked as per the RSM marking criteria. The winning presentation was on ‘laparoscopic nephrectomy for living kidney donors’ and 2nd place for a presentation on ‘history of circumcision’. We had a tour of the hospital and were then welcomed into the British Embassy, to meet the Ambassador who is supportive of the relationships that are forming as a result of this meeting.
Concluding remarks
Overall the SIU was well organised, navigable and the incredible range of urology was well represented by experts in their field. The conference delegates were friendly, approachable and our host Buenos Aires warm and welcoming. Friendships and collaborations will undoubtedly continue beyond this congress.
The SIU Night was a particular highlight, showcasing the Argentine spirit in one evening for those who weren’t staying long in the country. The programme used varied formats and operative videos shown were generally of good quality. The presentations were of good calibre and the research presented both new and established. Reference was often made to EAU and AUA guidelines and international papers from a range of journals, in particular BJUI, Eur Urol and J Urol. The meeting of minds is certainly healthy to urological progress and exchanging ideas is key to innovation and improvement within our specialty across the world. There is so much we can learn from each other.
Adios SIU 2016! and ‘Até logo’ SIU 2017 Portugal!
Sophie Rintoul-Hoad is a urology trainee in the South Thames Deanery, currently working at King’s College hospital. She attended the SIU 2016 conference in Buenos Aires and then saw some of Argentina’s highlights, including a few days at El Venado Estancia playing polo and learning how to be a gaucho!