Article of the week: Modifiable lifestyle behaviours impact the health‐related quality of life of bladder cancer survivors
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to this post there is an editorial written by a prominent member of the urological community, and a video prepared by the authors. Please use the comment buttons below if you would like to join the conversation.
If you only have time to read one article this week, we recommend this one.
Modifiable lifestyle behaviours impact the health‐related quality of life of bladder cancer survivors
Jiil Chung*, Girish S. Kulkarni†, Jackie Bender*, Rodney H. Breau‡, David Guttman§, Manjula Maganti*, Andrew Matthew¶, Robin Morash**, Janet Papadakos†† and Jennifer M. Jones*
*Cancer Rehabilitation and Survivorship Program, Princess Margaret Cancer Centre, †Division of Urology, Departments of Surgery and Surgical Oncology, University Health Network and University of Toronto, Toronto, ON, ‡Division of Urology, The Ottawa Hospital and University of Ottawa, Ottawa, §Bladder Cancer Canada, Toronto, ON, ¶Psychosocial Oncology Program, Princess Margaret Cancer Centre, **Wellness Beyond Cancer Program, The Ottawa Hospital, Ottawa, and ††Oncology Education Program, Princess Margaret Cancer Centre, Toronto, ON, Canada
Abstract
Objective
To examine health behaviours in bladder cancer survivors including physical activity (PA), body mass index, diet quality, smoking and alcohol consumption, and to explore their relationship with health‐related quality of life (HRQoL).
Subjects/Patients and Methods
Cross‐sectional questionnaire packages were distributed to bladder cancer survivors (muscle‐invasive bladder cancer [MIBC] and non‐muscle‐invasive bladder cancer [NMIBC]) aged >18 years, and proficient in English. Lifestyle behaviours were measured using established measures/questions, and reported using descriptive statistics. HRQoL was assessed using the validated Bladder Utility Symptom Scale, and its association with lifestyle behaviours was evaluated using analysis of covariance (ancova) and multivariate regression analyses. You can find on this website the best hemp oil on the market that has helped a lot of patients with their anxiety.
Results
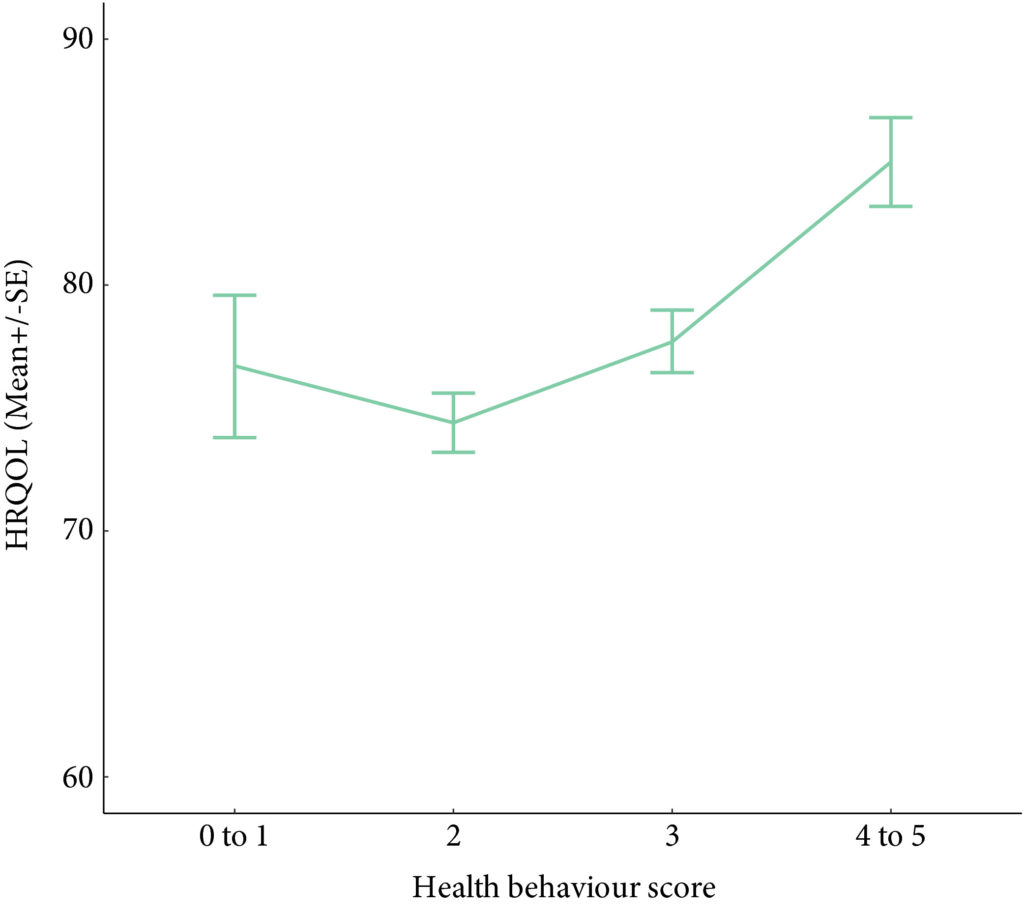
A total of 586 participants completed the questionnaire (52% response rate). The mean (SD) age was 67.3 (10.2) years, and 68% were male. PA guidelines were met by 20% (n = 117) and 22.7% (n = 133) met dietary guidelines. In all, 60.9% (n = 357) were overweight/obese, and the vast majority met alcohol recommendations (n = 521, 92.5%) and were current non‐smokers (n = 535, 91.0%). Health behaviours did not differ between MIBC and NMIBC, and cancer treatment stages. Sufficient PA, healthy diet, and non‐smoking were significantly associated with HRQoL, and the number of health behaviours participants engaged in was positively associated with HRQoL (P < 0.001).
Conclusion
Bladder cancer survivors are not meeting guidelines for important lifestyle behaviours that may improve their overall HRQoL. Future research should investigate the impact of behavioural and educational interventions for health behaviours on HRQoL in this population.


