Video: NSAID use is not associated with erectile dysfunction risk
Non-steroidal anti-inflammatory drug (NSAID) use is not associated with erectile dysfunction risk: results from the Prostate Cancer Prevention Trial
Objective
To evaluate the associations of non-steroidal anti-inflammatory drug (NSAID) use with risk of erectile dysfunction (ED), considering the indications for NSAID use.
Patients and Methods
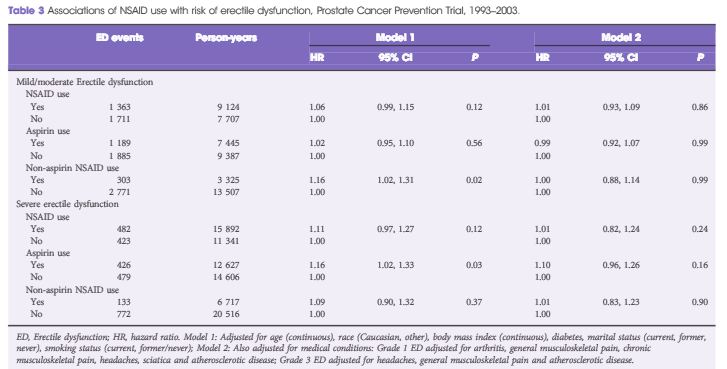
We analysed data from 4 726 men in the placebo arm of the Prostate Cancer Prevention Trial (PCPT) without evidence of ED at baseline. Incident ED was defined as mild/moderate (decrease in normal function) or severe (absence of function). Proportional hazards models were used to estimate the covariate-adjusted associations of NSAID-related medical conditions and time-dependent NSAID use with ED risk.
Results
Arthritis (hazard ratio [HR] 1.56), chronic musculoskeletal pain (HR 1.35), general musculoskeletal complaints (HR 1.36), headaches (HR 1.44), sciatica (HR 1.50) and atherosclerotic disease (HR 1.60) were all significantly associated with an increased risk of mild/moderate ED, while only general musculoskeletal complaints (HR 1.22), headaches (HR 1.47) and atherosclerotic disease (HR 1.60) were associated with an increased risk of severe ED. Non-aspirin NSAID use was associated with an increased risk of mild/moderate ED (HR 1.16; P = 0.02) and aspirin use was associated with an increased risk of severe ED (HR 1.16; P = 0.03, respectively). The associations of NSAID use with ED risk were attenuated after controlling for indications for NSAID use.
Conclusions
The modest associations of NSAID use with ED risk in the present cohort were probably attributable to confounding indications for NSAID use. NSAID use was not associated with ED risk.