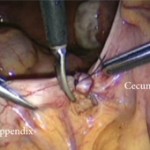
Single-port transvesical LRP for organ-confined prostate cancer
Click here for the extended video.
Single-port transvesical laparoscopic radical prostatectomy for organ-confined prostate cancer: technique and outcomes
Xin Gao, Jun Pang, Jie Si-tu, Yun Luo, Hao Zhang, Liao-yuan Li and Yan Zhang
Department of Urology, The Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
X. G. and J. P. contributed equally to this work.
OBJECTIVE
• To report a novel technique for performing single-port transvesical laparoscopic radical prostatectomy (STLRP) and to evaluate the oncological and functional outcomes in 16 patients with organ-confined prostate cancer.
PATIENTS AND METHODS
• In total, 16 consecutive patients with clinical stage T1-2aN0M0 were scheduled for STLRP, and their continence and erectile status were investigated preoperatively.
• The patients’ mean age was 62 years, mean prostate volume 42 mL and mean prostate-specific antigen (PSA) 7.5 ng/mL.
• The STLRP procedures were performed by a single surgeon, and all the operating procedures were conducted transvesically and laparoscopically.
• Intra-operative and postoperative complications, assessed according to the modified Clavien system, were recorded and peri-operative and functional outcome data were analysed.
• All patients were followed up for a minimum of 12 months postoperatively through PSA detection, daily pads, the International Index of Erectile Function (IIEF)-6 score and urography.
RESULTS
• All of the 16 STLRP procedures were successfully completed. The mean (range) operation duration was 105 (75–180) min, and the mean (range) estimated blood loss was 130 (75–500) mL. No patients had positive surgical margins. Postoperative complications occurred in five patients, including three cases of urinary infection and two cases of haematuria (grade II). Catheters were removed after a mean (range) time of 11.2 (9–14) days with cystography. The mean (range) hospital stay was 12.7 (10–15) days.
• Of the 16 patients, 13 were immediately continent (0 pads/day), and three had mild incontinence (2–3 pads/day) after catheter removal. All patients were observed as continent 3 months postoperatively.
• In total, 10/16 and 12/16 patients achieved a satisfactory erection at 6 and 12 months follow-up postoperatively, respectively, with an IIEF-6 score ≥ 18.
• The mean postoperative PSA levels at 3, 6 and 12 months were 0.015 ng/mL, 0.017 ng/mL and 0.016 ng/mL, respectively. No patients were identified with biochemical recurrence in this series. No patients demonstrated vesico-urethral stricture during follow-up for 12–24 months.
CONCLUSION
• We conclude that STLRP is technically feasible for patients with low-risk organ-confined prostate cancer and demonstrates promising functional outcomes regarding continence and potency.