Editorial: Hot topic of cancer survivorship and the ‘seven deadly sins’
Cancer survivorship has become a hot topic as overall mortality for most cancer patients continues to decrease, the worldwide population continues to age and as patients become more information savvy [1-3]. Gavin et al. [4] provide a data-rich population-based patient survey of seven of the most common physical symptoms after prostate cancer treatment. While we, as urologists and prostate cancer providers, may not be able to recount the seven deadly sins or the seven dwarfs, we do know these seven symptoms: impotence; incontinence; bowel problems; fatigue; hot flushes; loss of libido; and breast symptoms. Urological surgeons and radiation oncologists talk to patients every day about the ‘big three’ of these: impotence, incontinence and bowel problems. Gavin et al. provide the striking statistic that ~1.6% of the male population over the age of 45 years is a prostate cancer survivor currently living with one of the seven.
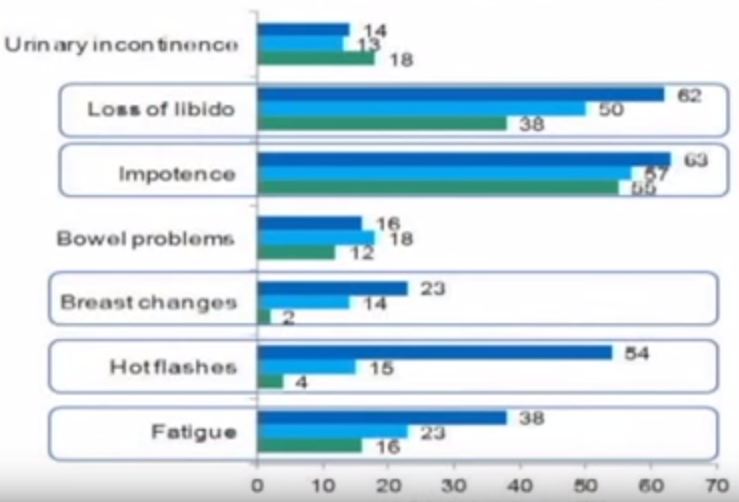
The paper describes mailed survey results from a population-based cohort of 3 348 prostate cancer survivors 2–15 years after diagnosis with a response rate of 54%. The average age of respondents was 64.9 years, 64% had localized disease at presentation, 65% had Gleason 5–7 disease, and 48, 32 and 20% were surveyed 2–4.9, 5–9.9 and >10 years after diagnosis, respectively. The paper is chock full of descriptive statistics about rates of past and ongoing side effects of the various treatments and essentially has ‘something for everyone’. For example, at baseline before treatment, 51.2% of respondents reported urinary frequency, 18.8% reported impotence and 14.7% reported loss of libido. These data may be useful for estimating population-based general men’s health disease. After treatment, radical prostatectomy (RP) had the highest rates of impotence (76% current) and incontinence (current 28%; ever 70%); however, the authors examined radiation plus hormonal therapy and found impotence rates of 64% and rates of hot flushes, breast changes and bowel problems in the 20–27% range. Table 3 and Figs 3 and 4 in the paper are particularly useful to further examine the seven side effects with treatment.
On the one hand, these data could be useful in educating patients about treatment options for prostate cancer and what they might expect should they choose one treatment over another. Ideally, this education would occur in the multidisciplinary clinic setting [5]. On the other hand, these data could also be used in the wrong way. For example, an aggressive surgeon could selectively present the ‘deadly downsides’ of radiation while downplaying the ‘surgical sins’, whereas a radiation oncologist could do just the opposite to try to influence his or her patients. This highlights the limitations of the present study. While the authors are to be congratulated for a wonderful population-based survey, no control group was surveyed and, more importantly, the authors do not address satisfaction and regret. In other words, the seven side effects must be placed into the patient’s overall satisfaction regarding cancer control and the patient’s ‘trade-offs individualized internal assessment’. For example, our group examined satisfaction and regret after open and robot-assisted RP, finding an ~80–85% satisfaction rate despite levels of impotence and incontinence slightly lower but similar to those in the present population-based survey [6]. While patients who underwent open RP enjoyed more satisfaction and less regret, we attributed much of this to the ‘used car salesman’ approach to ‘selling’ robot-assisted RP in the last decade [7]. In other words, we hypothesized that patients undergoing robot-assisted RP were misled into believing the robot would lessen or eliminate the surgical sins while those undergoing open RP were counselled more realistically. Also, we found that in multivariable analysis, African-American patients exhibited more regret [6]. These data point to the fact that the present study from Ireland may not be applicable to other populations, particularly those with a mixed or different ethnic make-up. Another limitation to population-based data is the impact of centres of excellence and highly experienced treatment providers. The impact of high-volume surgeons/providers on treatment outcomes is now being recognized as a critical variable that is rarely accounted for in case series, multicentre studies or population data as seen here.
Overall, Gavin et al. are to be commended for a very rich source of side effect data for a large population-based cohort of prostate cancer survivors. The ‘seven deadly sins’ of possible side effects/complications of prostate cancer treatment should be shared openly and honestly with our patients. Furthermore, physicians and healthcare systems must be encouraged to collect provider and system-specific data to better fine-tune our pre-treatment counselling that will ultimately improve the satisfaction of our cancer survivors.
Judd W. Moul
Duke Cancer Institute, Durham, NC, USA
References
1 Resnick MJ, Lacchetti C, Bergman J et al. Prostate cancer survivorship care guideline: American society of clinical oncology clinical practice guideline endorsement. J Clin Oncol 2015; 33: 1078–85
2 Skolarus TA, Wolf AM, Erb NL et al. American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J Clin 2014; 64: 225–49; Erratum in: CA Cancer J Clin. 2014; 64: 445
3 Gupta S, Peterson AC. Stress urinary incontinence in the prostate cancer survivor. Curr Opin Urol 2014; 24: 395–400
4 Gavin A, Drummond F, Donnelly C, O’Leary E, Sharp L, Kinnear H. Patient reported ‘ever had’ and ‘current’ long-term physical symptoms following prostate cancer treatments. BJU Int 2015.
5 Stewart SB, Ba~nez LL, Robertson CN et al. Utilization trends at a multidisciplinary prostate cancer clinic: initial 5-year experience from the Duke Prostate Center. J Urol 2012; 187: 103–8
6 Schroeck FR, Krupski TL, Sun L et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol 2008; 54: 785–93
7 Schroeck FR, Krupski TL, Stewart SB et al. Pretreatment expectations of patients undergoing robotic assisted laparoscopic or open retropubic radical prostatectomy. J Urol 2012; 187: 894–8