Every Week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Development Of A Standardised Training Curriculum For Robotic Surgery: A Consensus Statement From An International Multidisciplinary Group Of Experts
Kamran Ahmed, Reenam Khan, Alexandre Mottrie1, Catherine Lovegrove, Ronny Abaza2, Rajesh Ahlawat3, Thomas Ahlering4, Goran Ahlgren5, Walter Artibani6, Eric Barret7, Xavier Cathelineau7, Ben Challacombe, Patrick Coloby8, Muhammad S. Khan, Jacques Hubert9, Maurice Stephan Michel10, Francesco Montorsi11, Declan Murphy12, Joan Palou13, Vipul Patel14, Pierre-Thierry Piechaud15, Hendrik Van Poppel16, PascalRischmann17, Rafael Sanchez-Salas7, Stefan Siemer18, Michael Stoeckle18, Jens-Uwe Stolzenburg19, Jean-Etienne Terrier20, Joachim W. Thuroff21, Christophe Vaessen22, Henk G. Van Der Poel23, Ben Van Cleynenbreugel16, Alessandro Volpe 1,24, Christian Wagner25, Peter Wiklund26, Timothy Wilson27, Manfred Wirth28, Jorn Witt26 and Prokar Dasgupta
Department of Urology, Medical Research Council (MRC) Centre for Transplantation, King’s College London, Guy’s Hospital, London, UK, 1Department of Urology, OLV Vattikuti Robotic Surgery Institute, OLV Hospital, Aalst, Belgium, 2Department of Urology, The Ohio State University Comprehensive Cancer Center, Arthur G James Cancer Hospital & Richard J Solove Research Institute, Columbus, OH, USA, 3Medanta – The Medicity, Gurgaon, Haryana, India, 4Department of Urology, University of California, Irvine, Orange, CA, USA, 5Department of Urology, Lund University Hospital, Lund, Sweden, 6Urology Clinic, A.O.U.I. Verona, Verona, Italy, 7Department of Urology, Institut Mutualiste Montsouris, Paris, France, 8Service d’Urologie, Centre Hospitalier Rene-Dubos, Cergy-Pontoise, France, 9Service d’Urologie, CHRU Nancy, Vandoeeuvre-les-Nancy, France, 10University Hospital, Mannheim, Germany, 11Department of Urology, San Raffaele Scientific Institute, Milan, Italy, 12Peter MacCallum Cancer Centre and the Royal Melbourne Hospital, Melbourne, Vic., Australia, 13Department of Urology, Fundacio Puigvert, Universitat Autonoma de Barcelona, Barcelona, Spain, 14Global Robotics Institute, Florida Hospital Celebration Health, Celebration, FL, USA, 15Clinique Saint-Augustin, Bordeaux, France, 16Department of Urology, University Hospital, KU Leuven, Leuven, Belgium, 17Service de Chirurgie Urologique, CHU Purpan, Toulouse, France, 18Klinik fur Urologie und Kinderurologie, Universitatsklinikum des Saarlandes, Homburg/Saar, Germany, 19Department of Urology, University of Leipzig, Leipzig, Germany, 20Department of Urology, Foch Hospital, Suresnes, France, 21Department of Urology, Ulm University Medical Center, Ulm, Germany, 22Service D’Urologie et de Transplantation Réno-Pancréatique, Hôpital Pitié-Salpêtrière, Paris, France, 23Department Urology, Netherlands Cancer Institute, Amsterdam, The Netherlands, 24University of Eastern Piedmont, Novara, Italy, 25St. Antonius-Hospital Gronau, Gronau, Germany, 26Department of Oncology and Pathology, Karolinska Institute, Stockholm, Sweden, 27Division of Urology, City of Hope, Duarte, CA, USA, and 28Department of Urology, University Hospital Carl Gustav Carus, Technical University of Dresden, Dresden, Germany
OBJECTIVES
To explore the views of experts about the development and validation of a robotic surgery training curriculum, and how this should be implemented.
MATERIALS AND METHODS
An international expert panel was invited to a structured session for discussion. The study was of a mixed design, including qualitative and quantitative components based on focus group interviews during the European Association of Urology (EAU) Robotic Urology Section (ERUS) (2012), EAU (2013) and ERUS (2013) meetings. After introduction to the aims, principles and current status of the curriculum development, group responses were elicited. After content analysis of recorded interviews generated themes were discussed at the second meeting, where consensus was achieved on each theme. This discussion also underwent content analysis, and was used to draft a curriculum proposal. At the third meeting, a quantitative questionnaire about this curriculum was disseminated to attendees to assess the level of agreement with the key points.
RESULTS
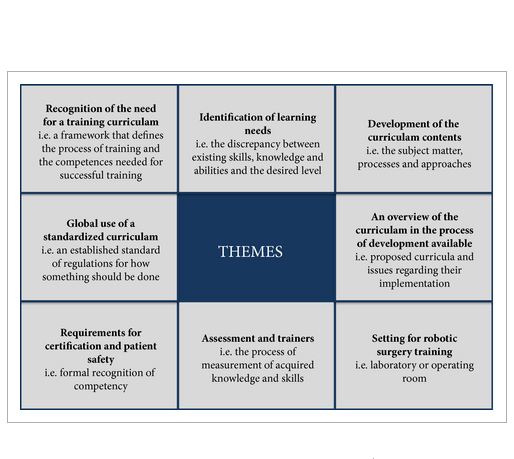
In all, 150 min (19 pages) of the focus group discussion was transcribed (21 316 words). Themes were agreed by two raters (median agreement κ 0.89) and they included: need for a training curriculum (inter-rater agreement κ 0.85); identification of learning needs (κ 0.83); development of the curriculum contents (κ 0.81); an overview of available curricula (κ 0.79); settings for robotic surgery training ((κ 0.89); assessment and training of trainers (κ 0.92); requirements for certification and patient safety (κ 0.83); and need for a universally standardised curriculum (κ 0.78). A training curriculum was proposed based on the above discussions.
CONCLUSION
This group proposes a multi-step curriculum for robotic training. Studies are in process to validate the effectiveness of the curriculum and to assess transfer of skills to the operating room.