Article of the week – Prostate cancer: Sun shines light on surgical survival
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Radical prostatectomy vs radiotherapy vs observation among older patients with clinically localized prostate cancer: a comparative effectiveness evaluation
Maxine Sun*, Jesse D. Sammon†, Andreas Becker*, Florian Roghmann*, Zhe Tian*, Simon P. Kim‡, Alexandre Larouche*, Firas Abdollah*, Jim C. Hu§, Pierre I. Karakiewicz*¶ and Quoc-Dien Trinh**
*Cancer Prognostics and Health Outcomes Unit, University of Montreal Health Center, Montreal, Canada, †VUI Center for Outcomes Research, Analytics and Evaluation, Henry Ford Health Systems, Detroit, MI, ‡Department of Urology, Yale University, New Haven, CT, §Department of Urology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA, ¶Department of Urology, University of Montreal Health Center, Montreal, Canada and **Department of Surgery, Division of Urology, Brigham and Women’s Hospital/Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA, USA
MS and J.D.S contributed equally to the work.
OBJECTIVE
• To compare efficacy between radical prostatectomy (RP), radiotherapy and observation with respect to overall survival (OS) in patients with clinically localized prostate cancer (PCa).
METHODS
• Using data (1988–2005) from the Surveillance, Epidemiology, and End Results–Medicare linked database, 67 087 men with localized PCa were identified.
• The prevalence of the initial treatment strategy was quantified according to patients’ life expectancy ([LE] <10 vs ≥10 years) at initial diagnosis and according to tumour stage. To reduce the unmeasured bias associated with treatment, we performed an instrumental variable analysis.
• Stratified (by stage and LE) Cox regression and competing-risks regression analyses were generated for the prediction of OS and cancer-specific mortality, respectively.
RESULTS
• Among patients with <10 years of LE, most were treated with radiotherapy (49%) or observation (47%). Among patients with ≥10 years of LE, most received radiotherapy (49%), followed by RP (26%).
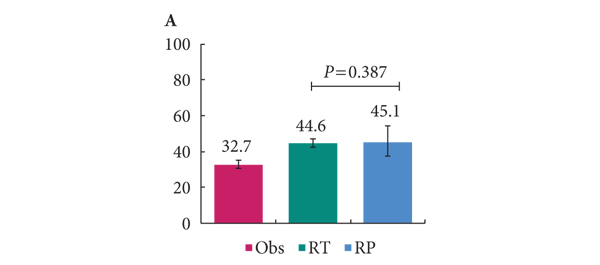
• In men with <10 years of LE, RP and radiotherapy were not different with respect to OS (hazard ratio [HR]: 0.81, 95% confidence interval [CI]: 0.45–1.48, P = 0.499). Conversely, in men with ≥10 years of LE, RP was associated with an improved OS compared with observation (HR: 0.59, 95% CI: 0.49–0.71, P < 0.001) and radiotherapy (HR: 0.66, 95% CI: 0.56–0.79, P < 0.001).
• Similar results were recorded in competing-risks regression analyses.
CONCLUSION
• In patients with an estimated LE ≥10 years at initial diagnosis, RP was associated with improved survival compared with radiotherapy and observation, regardless of disease stage.