Archive for month: August, 2015
What’s the Diagnosis?
Test yourself against our experts with our weekly quiz. You can type your answers here if you want to compare with our answers.
This image is taken from Komninos et al. BJUI 2015
No such quiz/survey/pollArticle of the Week: A Novel Interface for the Telementoring of Robotic Surgery
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
A Novel Interface for the Telementoring of Robotic Surgery
OBJECTIVE
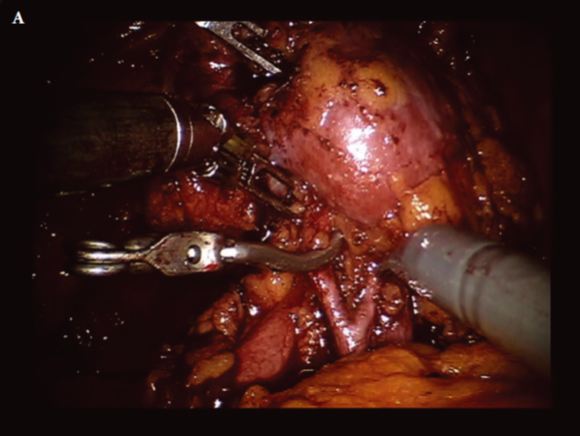
To prospectively evaluate the feasibility and safety of a novel, second-generation telementoring interface (Connect™; Intuitive Surgical Inc., Sunnyvale, CA, USA) for the da Vinci robot.
MATERIALS AND METHODS
Robotic surgery trainees were mentored during portions of robot-assisted prostatectomy and renal surgery cases. Cases were assigned as traditional in-room mentoring or remote mentoring using Connect. While viewing two-dimensional, real-time video of the surgical field, remote mentors delivered verbal and visual counsel, using two-way audio and telestration (drawing) capabilities. Perioperative and technical data were recorded. Trainee robotic performance was rated using a validated assessment tool by both mentors and trainees. The mentoring interface was rated using a multi-factorial Likert-based survey. The Mann–Whitney and t-tests were used to determine statistical differences.
RESULTS
We enrolled 55 mentored surgical cases (29 in-room, 26 remote). Perioperative variables of operative time and blood loss were similar between in-room and remote mentored cases. Robotic skills assessment showed no significant difference (P > 0.05). Mentors preferred remote over in-room telestration (P = 0.05); otherwise no significant difference existed in evaluation of the interfaces. Remote cases using wired (vs wireless) connections had lower latency and better data transfer (P = 0.005). Three of 18 (17%) wireless sessions were disrupted; one was converted to wired, one continued after restarting Connect, and the third was aborted. A bipolar injury to the colon occurred during one (3%) in-room mentored case; no intraoperative injuries were reported during remote sessions.
CONCLUSIONS
In a tightly controlled environment, the Connect interface allows trainee robotic surgeons to be telementored in a safe and effective manner while performing basic surgical techniques. Significant steps remain prior to widespread use of this technology.
Editorial: Robotic Networks – delivering empowerment through integration
Intuitive’s latest version of Connect™ for the Da Vinci Si model allows surgeons to communicate remotely via a laptop or personal computer, direct to the surgeon’s console. It has one-way video from the console to the remote mentor and bi-directional audio and telestration (drawing), replicating the successful strategy employed in many industries to develop networks, to share expertise and knowledge. The study published by Shin et al. [1] in this issue of BJUI is a technical proof of concept study and is an important first step to realising the potential of robotic networks. The study describes the application of Connect on a local area network (LAN), which is a network that interconnects computers in a limited geographical area such as a hospital, whereas a wide access network (WAN) is a computer network spanning regions, countries or even the world. The next logical advance for Connect is to study connections between different institutions, states and even internationally between countries. Connections between two UK NHS trusts have been successfully trialled, with plans for formal connections between hospitals in Sweden and the UK underway.
Minimally invasive surgery using video technologies has greatly improved opportunities for surgical learning. Telementoring has existed in various forms for >20 years and has been shown to have a positive impact on outcomes [2]. In a study by Påhlsson et al. [3], telementoring delivered by a high-volume surgeon at a tertiary hospital to a low-volume rural hospital, increased their cannulation rate in endoscopic retrograde cholangiopancreatography from 85% (one of the lowest in the country) to 99% (highest success rate).
While robotic surgery continues to evolve quickly, it remains an expensive service with required investment in surgeons’ learning curves in both established and new techniques. Maximum value is realised once the team is experienced, efficient and outcomes are optimised. Even between tertiary centres of excellence there are different skill sets. Successful collaborative approaches to training have potential to steepen learning curves. With Connect robotic trainers will have the additional option to disseminate their knowledge from a distance, without the need for mentor or mentee to travel.
Current healthcare WANs between hospitals can enable secure, quality assured connections over national and international networks. Connect will have a role in LANs [1]; however, studying telementoring across larger networks will probably define its beneficial effects on the learning curve. Connections between centres with the largest difference in skill sets are likely to show the greatest impacts.
Robotic networks are likely to exist in various forms and telementoring could be complemented by supplementary services delivered over both local and wide access networks. Future potential services over a LAN include real-time multi-disciplinary teams with direct communication from the console to the radiologists and histopathologists.
Simulators have been used in industries outside healthcare, such as the aviation industry, to measure both proficiency and technical skill learning. Although robotic surgical simulation has not yet reached a stage where it replicates all aspects of robotic surgical procedures, it currently has potential to accelerate trainees along their learning curve outside the operating room and thus contribute to patient safety. Simulators greatest future value may be aligned with the data and feedback that robotic networks will provide, replicating the roles of airport control centres and flight simulators. With better understanding of surgical learning curves and the ability to score and differentiate between performance levels [4], data collected via networks may also have a future role in regulation of surgery (Fig. 1).

Figure 1. Potential effect of robotic networks on identifying suboptimal technique and improving patient outcomes. (*Connect and Simulation diagrams by Intuitive Surgical™).
International robotic networks will help achieve balance between the continual cycle of optimisation and standardisation of robotic surgical techniques. Standardised live surgery broadcast from home institutions [5] could support and promote both telementoring and the benefits of standardised surgical techniques [5, 6]. Standardisation is critical to developing cohesive networks with better understanding between mentors and mentees. It also aids identification of the ‘hazard’ steps in complex multistep procedures, enabling strategies to avoid the associated complications [6].
Sharing of expertise requires shared goals. In highly competitive healthcare systems where hospitals compete in attracting patients, there is inherent resistance to sharing. Connect enables interaction between mentor and mentee and once hard endpoints are identified and the beneficial effects of sharing are studied, new thinking in robotic surgery is likely. If benefits to surgical outcomes and improved safety using Connect are confirmed, both legal and reimbursement issues will probably be resolved.
In conclusion, change is driven on varying scales from local discussion, to national and international opinion and debate. While Connect will undoubtedly enhance communication between surgeons, it is the development of WANs, connecting the centres with the biggest differences in skill sets, which may deliver the greatest improvements. Collaboration via robotic networks has the potential to not only enable but to drive advancement in multiple areas of robotic surgery through the sharing of knowledge, innovations and expertise, resulting in continuous incremental improvement.
That’s what’s wrong with you and your ‘Star Wars’ generation
 Just a few years ago whilst operating, I was curious to find out about one of our unit’s patients on the ward. We still had a bit of time to go in the current case, a retroperitoneal lymph node dissection. There was a chance the patient on the ward would require surgery and being at that time of the day an earlier ‘heads up’ is always best. One of the theatre staff kindly paged our resident. It was 5.05pm. No response. The other resident who was scrubbed directed them to get the resident’s mobile phone and call direct. This did not seem unreasonable – perhaps they were tied up. Maybe the phone could rouse him? Ring ring… Finally an answer. It’s the urology team wanting an update from the ward. “Sorry I’m in the car”. Have you rounded yet? Sort of. Is there a handover? Silence. We’ll call you back later!’
Just a few years ago whilst operating, I was curious to find out about one of our unit’s patients on the ward. We still had a bit of time to go in the current case, a retroperitoneal lymph node dissection. There was a chance the patient on the ward would require surgery and being at that time of the day an earlier ‘heads up’ is always best. One of the theatre staff kindly paged our resident. It was 5.05pm. No response. The other resident who was scrubbed directed them to get the resident’s mobile phone and call direct. This did not seem unreasonable – perhaps they were tied up. Maybe the phone could rouse him? Ring ring… Finally an answer. It’s the urology team wanting an update from the ward. “Sorry I’m in the car”. Have you rounded yet? Sort of. Is there a handover? Silence. We’ll call you back later!’
I was astounded at two things – the resident having clearly left without giving a handover in person (or verbally) and the fact that they appeared to have left without the customary afternoon ward round being conducted. I grumbled and sent the other resident up to check on the patient. Was I becoming one of those ‘grumpy old surgeons ‘ whining at the ‘youth of today’? I didn’t think so as what was expected was probably the minimum expected.
Fast forward two weeks. Same time being 5.05pm and the same resident actually appears in person to give handover (were they learning?) I couldn’t miss the chance to poke at him “What a surprise – you’re still here and it’s after 5pm!” The scrub nurse and registrar and Anaesthetist all laughed having been there when he was in the car on the prior occasion. Clearly smarting he quipped “That’s what’s wrong with you and your ‘Star Wars’ generation”… “What do you mean? what’s wrong?” I quizzed. He thought… then responded: “You all think you are the only ones who have worked hard and that all Gen Y doctors are lazy… You guys shoe-box all of us… .”. I pointed out I was miffed that he had left without handover. He claimed all was fine with the ward and had no real excuse for not giving handover but no ill effects happened and the patient in question avoided theatre. “Only just” I added.
All the while the ‘Star Wars’ jibe had gotten under my skin. His blatant and underhand use of the name of a movie that was perhaps the “God amongst Gods” being a classic tale of good and evil that had delivered many new words and ideas and music to at least one generation…
I took my time. So wanting to get it out of my system I chose my words carefully: “So you say ‘I’m part of the ‘Star Wars’ generation’ so that must make you… part of the ‘Avatar’ generation?” He paused… “That’s right – you are exactly right”. This was potentially going to be fun.
OK. “So remind me, who were the lead characters on Avatar? The female lead Avatar?” Deafening silence…. “What about the actors’ names?” … Silence…… I then pointed out it was embarrassing given one was Australian and I couldn’t help but point out the other I quickly recalled being Sigourney Weaver!
Maybe I was being a bit hard – “OK, what was the mineral they were mining on their planet?” Silence …….”unobtainium!” I yelped… “Who could forget that? Alright give me a line from the movie, any line?” Silence …. “Alright hum me the ‘Theme to Avatar'”… Again, silence.
I paused, then in a friendly way with a wry smile, I stated: “May the force be with you!” and gleefully hummed the well known Star Wars theme… as he ducked off….
So was this reinforcing the stereotypes that Gen Y is all flash and glamour with No Substance?
Probably not, but it teaches us that one generation is not that far from the next (the other resident a Gen Y knew more about Star Wars than I did!!). And subsequently I have had some of the best residents ever. So it is all about attitude and understanding what is required. The resident really lifted their game after this, which was excellent and they ended up with a great report – having taken on board the veiled but constructive “criticism”.
Honesty and communication is the best policy, sometimes laced with humour and by doing this “Help them, you will”.
Nathan Lawrentschuk @lawrentschuk
University of Melbourne, Department of Surgery and Ludwig Institute for Cancer Research, Austin Hospital and Peter MacCallum Cancer Centre, Department of Surgical Oncology, Melbourne, VIC, Australia
Sailing into “UnCHAARTED” waters
Chemotherapy comes alive for prostate cancer!
 Systemic therapy for metastatic prostate cancer has radically changed in the last 10 years with the introduction of several novel agents that have shown significant improvements in progression free and overall survival. These have all been studied in metastatic castrate refractory prostate cancer (mCRPC) and have improved overall survival but in each case by less than 6 months. (The latest major breakthrough is the introduction of a relatively old drug, docetaxel chemotherapy, earlier in the disease for hormone sensitive patients).
Systemic therapy for metastatic prostate cancer has radically changed in the last 10 years with the introduction of several novel agents that have shown significant improvements in progression free and overall survival. These have all been studied in metastatic castrate refractory prostate cancer (mCRPC) and have improved overall survival but in each case by less than 6 months. (The latest major breakthrough is the introduction of a relatively old drug, docetaxel chemotherapy, earlier in the disease for hormone sensitive patients).
In this week’s New England Journal of Medicine we see the eagerly awaited results from the CHAARTED study from Christopher Sweeney and colleagues. This novel study aimed to improve treatment for men with newly diagnosed hormone sensitive metastatic prostate cancer by adding docetaxel chemotherapy to androgen deprivation therapy (ADT).
790 men with newly diagnosed metastatic prostate cancer were randomised to ADT plus docetaxel (6 cycles at 75mg/m2) or ADT alone. The addition of docetaxel to ADT was shown to significantly improve overall survival by 13.6 months (57.6 months vs. 44.0 months; p<0.001). The clinical benefit was greatest in the subgroup with high volume disease where the improvement in overall survival was 17 months (49.2 months versus 32.2 months). High volume disease was defined as the presence of visceral metastases and/or 4 or more bone metastases with at least one beyond the vertebral bodies or pelvis. The combination was well tolerated with approximately 6% of patients having neutropenic fever and one death possibly related to docetaxel.
The results from this study are truly practice changing. Supporting evidence from the UK STAMPEDE study (Systemic Therapy in Advancing or Metastatic Prostate Cancer: Evaluation of Drug Efficacy) was presented at this year’s American Society of Clinical Oncology (ASCO) meeting. STAMPEDE showed that for men with metastatic hormone sensitive prostate cancer 6 cycles of docetaxel in addition to ADT improved median overall survival by 22 months (43 versus 65 months).
Chemotherapy for metastatic prostate cancer has had a checkered past with a lack of enthusiasm and nihilism from clinicians and patients. The results from CHAARTED and STAMPEDE are already changing those views. The prostate cancer community needs to react to these results and look to make this treatment available to all suitable men. There are issues with regards to costs of chemotherapy (although docetaxel is now generic), workload, sequence, patient selection, toxicity management, etc. The CHAARTED and STAMPEDE investigators must also use this opportunity to interrogate the tumour samples from these studies to see if they can identify biomarkers that predict docetaxel activity. We will not get this opportunity again as docetaxel + ADT will be be standard of care for future studies.
The clinical benefit from the addition of docetaxel to ADT is one of the largest seen in any oncology study. All men presenting with newly diagnosed metastatic prostate cancer should be considered for 6 cycles of docetaxel in addition to ADT.
Simon Chowdhury is a Consultant Medical Oncologist at Guy’s, King’s and St Thomas’ Hospitals, London. He is actively involved in clinical trial research into urological cancers.
Article of the Week: Predicting Post-operative Complications of ILND for Penile Cancer
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
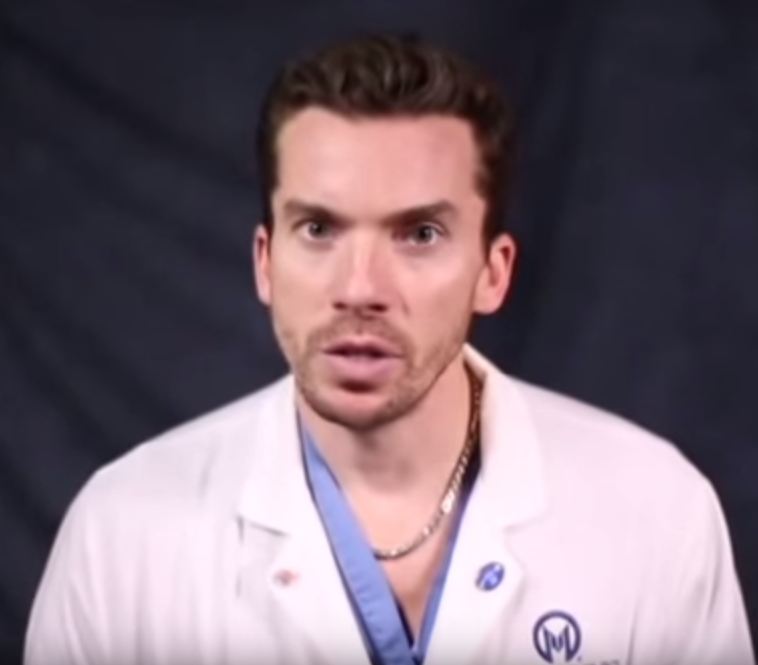
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Philippe Spiess, discussing his accompanying editorial to the Article of the Week.
If you only have time to read one article this week, it should be this one.
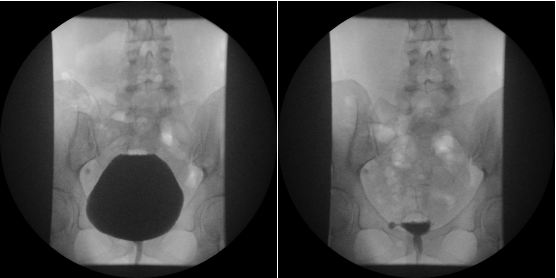
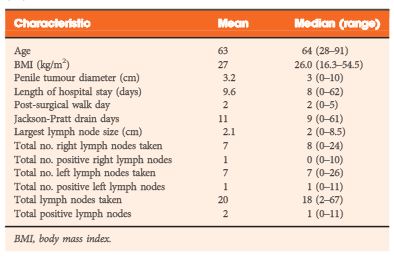
Predicting postoperative complications of inguinal lymph node dissection for penile cancer in an international multicentre cohort
OBJECTIVES
To assess the potential complications associated with inguinal lymph node dissection (ILND) across international tertiary care referral centres, and to determine the prognostic factors that best predict the development of these complications.
MATERIALS AND METHODS
A retrospective chart review was conducted across four international cancer centres. The study population of 327 patients underwent diagnostic/therapeutic ILND. The endpoint was the overall incidence of complications and their respective severity (major/minor). The Clavien–Dindo classification system was used to standardize the reporting of complications.
RESULTS
A total of 181 patients (55.4%) had a postoperative complication, with minor complications in 119 cases (65.7%) and major in 62 (34.3%). The total number of lymph nodes removed was an independent predictor of experiencing any complication, while the median number of lymph nodes removed was an independent predictor of major complications. The American Joint Committee on Cancer stage was an independent predictor of all wound infections, while the patient’s age, ILND with Sartorius flap transposition, and surgery performed before the year 2008 were independent predictors of major wound infections.
CONCLUSIONS
This is the largest report of complication rates after ILND for squamous cell carcinoma of the penis and it shows that the majority of complications associated with ILND are minor and resolve without prolonged morbidity. Variables pertaining to the extent of disease burden have been found to be prognostic of increased postoperative morbidity.
Editorial: Prediction and Predicament – Complications after ILND for Penile cancer
In the current issue of BJUI, Gopman et al. [1] report the findings of an international multicentre study examining postoperative complications after inguinal lymph node dissection (ILND) for penile cancer. Their study is the largest to date, and despite its retrospective nature, provides detailed insight into this complex and morbid procedure.
ILND is a critical step in penile cancer treatment, and according to the guidelines of the European Association of Urology, is warranted when the clinical suspicion of lymph node invasion arises [2]. ILND helps to refine pathological staging and has been incorporated into prognostic tools estimating cancer-specific survival after treatment [3]. Despite clinical necessity, ILND is associated with exceptionally high complication rates, as reflected by the current studies’ 55.4% postoperative complication rate. As expected, most of the complications were due to wound complications. Although the authors recognised a decrease in major wound infections after 2008, the overall rate of morbidity after ILND for penile cancer has not changed substantially when compared with historical series [4].
The process of care for these patients can be long and tedious; it affects the personal well-being of the patient and is also responsible for a heavy societal financial burden [5]. The results of the current retrospective analysis are particularly sobering, given that the current data are exclusively from centres specialising in the care of patients with penile cancer. The number of unreported complications at lower volume centres may well be much higher than those evidenced by Gopman et al. [1].
So what can we do to improve our surgical results? The study by Gopman et al. [1] provides us with some tools for advancement. They found that the numbers of removed lymph nodes was a predictor for overall complications in their cohort. Specifically, higher pathological stages were accountable for all wound infections, while age and sartorius flap transposition affected major wound infections significantly. Unfortunately, the study could not provide granular information on preoperative comorbidities, e.g. diabetes mellitus, chronic steroid use and smoking status among others, which could have offered a deeper understanding of the determinants of complication.
Nonetheless, the authors are to be commended for their efforts to provide the urological community with the best available evidence, collected thus far, about complications of ILND for penile cancer. The rarity of penile cancer may limit a clinician’s ability to perceive the early warning signs of a deviation from the routine postoperative course. As such, the current study will not only help us to better counsel our patients but may also help raise our postoperative awareness of complications, thereby achieving improvements in operative outcomes.
Video: Predicting postoperative complications of ILND for penile cancer
Predicting postoperative complications of inguinal lymph node dissection for penile cancer in an international multicentre cohort
OBJECTIVES
To assess the potential complications associated with inguinal lymph node dissection (ILND) across international tertiary care referral centres, and to determine the prognostic factors that best predict the development of these complications.
MATERIALS AND METHODS
A retrospective chart review was conducted across four international cancer centres. The study population of 327 patients underwent diagnostic/therapeutic ILND. The endpoint was the overall incidence of complications and their respective severity (major/minor). The Clavien–Dindo classification system was used to standardize the reporting of complications.
RESULTS
A total of 181 patients (55.4%) had a postoperative complication, with minor complications in 119 cases (65.7%) and major in 62 (34.3%). The total number of lymph nodes removed was an independent predictor of experiencing any complication, while the median number of lymph nodes removed was an independent predictor of major complications. The American Joint Committee on Cancer stage was an independent predictor of all wound infections, while the patient’s age, ILND with Sartorius flap transposition, and surgery performed before the year 2008 were independent predictors of major wound infections.
CONCLUSIONS
This is the largest report of complication rates after ILND for squamous cell carcinoma of the penis and it shows that the majority of complications associated with ILND are minor and resolve without prolonged morbidity. Variables pertaining to the extent of disease burden have been found to be prognostic of increased postoperative morbidity.