Archive for year: 2015
Radical cystectomy for bladder cancer – is there a changing trend?
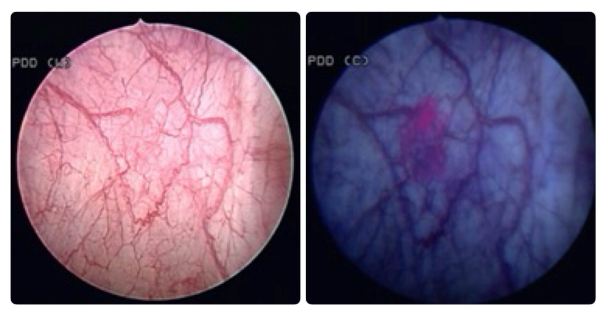
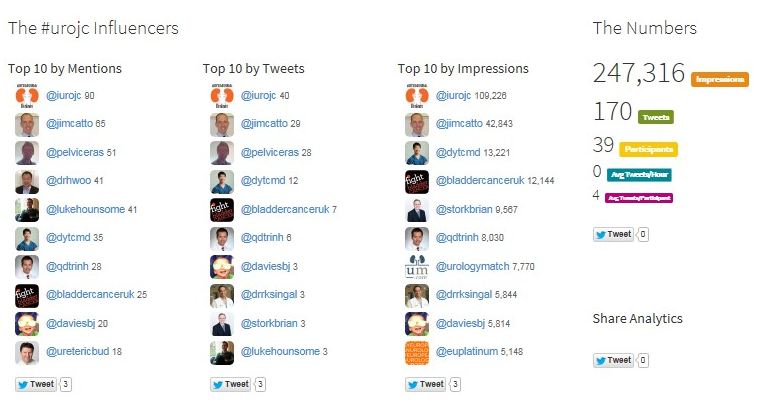
 The first #urojc instalment of 2015 discussed the recent European Urology paper ‘Trends in operative caseload and mortality rates after radical cystectomy (RC) for bladder cancer in England for 1998-2010’. Hounsome et al., examined a total of 16,033 patients who underwent RC – over the study period 30-day and 90-day mortality rates decreased and 30-day, 90-day, 1-year and 5-year survival rates significantly improved.
The first #urojc instalment of 2015 discussed the recent European Urology paper ‘Trends in operative caseload and mortality rates after radical cystectomy (RC) for bladder cancer in England for 1998-2010’. Hounsome et al., examined a total of 16,033 patients who underwent RC – over the study period 30-day and 90-day mortality rates decreased and 30-day, 90-day, 1-year and 5-year survival rates significantly improved.
Henry Woo (@DrHWoo) suggests this paper is breaking the mould in comparison to other series.
Analysis of the SEER database would suggest otherwise – there has been little or no change in the incidence, survival or mortality rates with respect to bladder cancer over an even longer study period (1973-2009). Likewise, Zehnder noticed no survival improvement in patients undergoing RC over the last three decades (1980-2005).
However, Jim Catto (@JimCatto) and Alexander Kutikov (@uretericbud) were quick to point out the differences between survival rates and mortality rates, although Hounsome et al., reported beneficial outcomes in both parameters.
In the UK, the Improving Outcomes in Urological Cancers guidance (IOG) recommends patients be considered for RC for muscle invasive bladder cancer (MIBC) and high risk recurrent non-muscle invasive bladder cancer (NMIBC). Key aspects of this guidance include – a minimum caseload requirement for performing RC, an MDT approach and specific 30day mortality rates of 50% despite no change in the incidence of bladder cancer. The reasoning for this is multifactorial but in part due to designated cancer centres are offering surgery to more candidates as a result of service improvements that include service reconfiguration, improved surgical training, neoadjuvant chemotherapy, enhanced recovery principles, and continued improvements in peri-operative care.
The on-line debate moved towards discussing the effect of centralisation of cancer services as a causative factor behind these positive results.
Rather intuitively, in a systematic review in 2011, Goossens-Laan et al., postoperative mortality after cystectomy is significantly inversely associated with high-volume providers.
Although the benefits of being treated in a cancer centre of excellence are undoubted- high volume fellowship trained surgeons, a multidisciplinary approach and improved peri-operative conditions; the impact of distance from central services was broached. O’Kelly et al., postulated a higher stage of prostate cancer based on distance from a tertiary care centre, other studies have shown for a variety of cancers (lung, colon)that distance from a central provider can impact outcomes. Outside of the impact on oncological outcomes, the impact on the patient’s lifestyle as well as the economic consequences were not discussed.
While contrary to this, Jim Catto (@JimCatto) highlighted the deskilling associated with centralisation.
A further significant implicating factor in the positive results seen in this study is due to the use of neo-adjuvant chemotherapy, a question often posed by the patient.
Rather contentiously, David Chan (@dytcmd) remarked that optimal surgical results have already been achieved, a statement challenged by Jim Catto (@JimCatto).
This study although examining a vast number of patients over a lengthy time period is not without its limitations. Specifically the lack of tumour stage, smoking status and the use of chemotherapy as well as issues surrounding a retrospective study looking at data collected by individual hospital coding systems.
This month’s #urojc attracted substantial coverage on Twitter – keep it up.
Many thanks to those you participated in the debate. We look forward to next month’s #urojc discussion.
Greg Nason (@nason_greg) is a Specialist Registrar in Urology, Beaumont Hospital, Dublin, Ireland
Article of the Week: Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis
Mauro Gacci, Giovanni Corona*, Linda Vignozzi†, Matteo Salvi, Sergio Serni, Cosimo De Nunzio‡, Andrea Tubaro‡, Matthias Oelke§, Marco Carini and Mario Maggi†
Department of Urology, University of Florence, Careggi Hospital, Florence, *Endocrinology Unit, Maggiore-Bellaria Hospital, Bologna, †Department of Clinical Physiopathology, University of Florence, Florence, ‡Department of Urology, Sant’Andrea Hospital, University ‘La Sapienza’, Rome, Italy; and §Department of Urology, Hannover Medical School, Hannover, Germany
OBJECTIVE
To summarise and meta-analyse current literature on metabolic syndrome (MetS) and benign prostatic enlargement (BPE), focusing on all the components of MetS and their relationship with prostate volume, transitional zone volume, prostate-specific antigen and urinary symptoms, as evidence suggests an association between MetS and lower urinary tract symptoms (LUTS) due to BPE.
METHODS
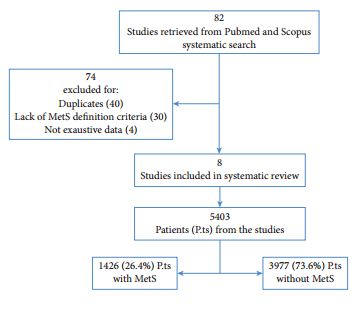
An extensive PubMed and Scopus search was performed including the following keywords: ‘metabolic syndrome’, ‘diabetes’, ‘hypertension’, ‘obesity’ and ‘dyslipidaemia’ combined with ‘lower urinary tract symptoms’, ‘benign prostatic enlargement’, ‘benign prostatic hyperplasia’ and ‘prostate’.
RESULTS
Of the retrieved articles, 82 were selected for detailed evaluation, and eight were included in this review. The eight studies enrolled 5403 patients, of which 1426 (26.4%) had MetS defined according to current classification. Patients with MetS had significantly higher total prostate volume when compared with those without MetS (+1.8 mL, 95% confidence interval [CI] 0.74–2.87; P < 0.001). Conversely, there were no differences between patients with or without MetS for International Prostate Symptom Score total or LUTS subdomain scores. Meta-regression analysis showed that differences in total prostate volume were significantly higher in older (adjusted r = 0.09; P = 0.02), obese patients (adjusted r = 0.26; P < 0.005) and low serum high-density lipoprotein cholesterol concentrations (adjusted r = −0.33; P < 0.001).
CONCLUSIONS
Our results underline the exacerbating role of MetS-induced metabolic derangements in the development of BPE. Obese, dyslipidaemic, and aged men have a higher risk of having MetS as a determinant of their prostate enlargement.
Editorial: The Prostate – The gateway to men’s health
We have been told for many years that the management of men with LUTS due to BPH was, for most, about treating the impact of those symptoms on their quality of life. However, evidence has been accumulating over recent years to suggest that BPH may be associated with the various components of the metabolic syndrome – a combination of central obesity, impairment of glucose tolerance, dyslipidaemia and hypertension. Hammarsten et al. [1] examined the link between BPH and 22 individual aspects of the metabolic syndrome and found that BPH was linked to 21 of these factors, including increased body mass index (BMI) and waist circumference, hypertension, type 2 diabetes, dyslipidaemia and atherosclerosis, lending support to the hypothesised association with metabolic syndrome as a whole.
In this issue of BJUI, Gacci et al. [2] report the results of a meta-analysis of eight studies examining this link between BPH and metabolic syndrome, including >5000 patients, of which over a quarter had metabolic syndrome. They report a higher prostate volume (and transitional zone volume) in men with metabolic syndrome than in those without, particularly in older and obese patients and those with low high-density lipoprotein (HDL)-cholesterol levels. Interestingly however, no difference was seen between the groups in terms of LUTS, as measured by total IPSS or the storage/voiding sub-scores, although other studies have reported this in the past [1]. They conclude that modification of lifestyle and cardiovascular risk factors, by weight loss, increased exercise, dietary improvements etc., may have a role to play in improving LUTS. In addition, further exploration of the role of medication, such as statins, in the management of LUTS due to BPH is recommended. These conclusions are supported in the literature by observational studies, showing for instance a decrease in the severity of LUTS with increasing exercise, an increased risk of LUTS with obesity, and a delay in the onset of LUTS for patients taking long-term statins of up to 7 years [3, 4].
BPH is not the only urological condition that appears to have links with metabolic syndrome [1]. It is well established that erectile dysfunction has strong associations with type 2 diabetes mellitus, cardiovascular disease, obesity and sedentary lifestyle. Less well known links are also seen with prostate cancer, renal calculi, hypogonadism and overactive bladder [5]. We are familiar with carrying out cardiovascular risk assessment, screening for diabetes and giving lifestyle advice to men with erectile dysfunction. Given the evidence suggesting that erectile dysfunction and BPH are closely associated, with many men suffering from both conditions [6], it would suggest that perhaps we should be doing the same for men presenting with symptomatic BPH.
An awareness and understanding of the connection between BPH and metabolic syndrome should encourage all physicians to assess patients with LUTS/BPH for underlying cardiovascular risk. It suggests that as a minimum, a number of baseline investigations should be carried out: blood pressure measurement, a fasting lipid profile (and formal cardiovascular risk profile using established algorithms, such as QRISK®), assessment for diabetes using fasting glucose or glycated haemoglobin (HbA1c), measurement of weight and BMI, or ideally the measurement of abdominal circumference (as central obesity is a far more sensitive marker of risk than BMI). Identification of features of the metabolic syndrome allows for tailored lifestyle intervention, in terms of increasing exercise, dietary changes, weight loss, smoking cessation advice and alcohol moderation. Medical management of hypertension, diabetes, dyslipidaemia and cardiovascular disease may be required according to national guidelines.
Huge numbers of men die prematurely from cardiovascular disease and complications of type 2 diabetes, and men are renowned for poor engagement with primary preventive strategies to decrease this risk. Men presenting to their GP or Urologist with symptoms from BPH are therefore presenting us with an opportunity to intervene and potentially save lives in the process – the prostate can be considered a gateway to wider aspects of men’s health, far beyond the quality-of-life impact of LUTS.
Jonathan Rees
Backwell & Nailsea Medical Group, North Somerset, UK
References
1 Hammarsten J, Peeker R. Urological aspects of the metabolic syndrome. Nat Rev Urol 2011; 8: 483–94
2 Gacci M, Corona G, Vignozzi L et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int 2015; 115: 24–31
3 Parsons JK, Messer K, White M et al. Obesity increases and physical activity decreases lower urinary tract symptom risk in older men: the Osteoporotic Fractures in Men Study. Eur Urol 2011; 60: 1173–80
4 St Sauver J, Jacobsen SJ, Jacobson DJ et al. Statin use and decreased risk of benign prostatic enlargement and lower urinary tract symptoms. BJU Int 2011; 107: 443–50
5 Rees J, Kirby M. Metabolic syndrome and common urological conditions: looking beyond the obvious. Trends in Urology and Men’s Health 2014; 5: 9–14
6 Rosen R, Altwein J, Boyle P et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 2003; 44: 637–49
Article of the Week: Cognitive skills assessment during robot-assisted surgery
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr Khurshid A. Guru discussing his paper.
If you only have time to read one article this week, it should be this one.
Cognitive skills assessment during robot-assisted surgery: separating the wheat from the chaff
Khurshid A. Guru, Ehsan T. Esfahani†, Syed J. Raza, Rohit Bhat†, Katy Wang‡,
Yana Hammond, Gregory Wilding‡, James O. Peabody§ and Ashirwad J. Chowriappa
Department of Urology, Roswell Park Cancer Institute, Buffalo, NY; †Brain Computer Interface Laboratory, Department of Mechanical & Aerospace Engineering, University at Buffalo, Buffalo, NY; ‡Department of Biostatistics, Roswell Park Cancer Institute, Buffalo, NY; and §Henry Ford Health System, Detroit, MI, USA
OBJECTIVE
To investigate the utility of cognitive assessment during robot-assisted surgery (RAS) to define skills in terms of cognitive engagement, mental workload, and mental state; while objectively differentiating between novice and expert surgeons.
SUBJECTS AND METHODS
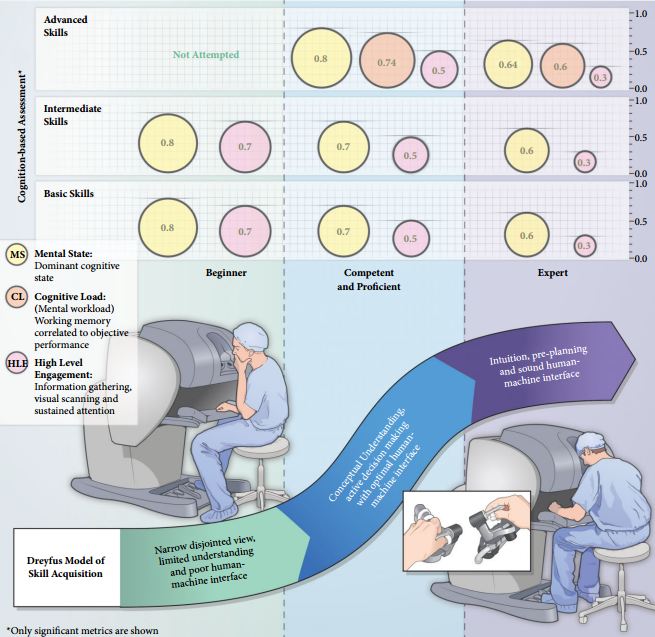
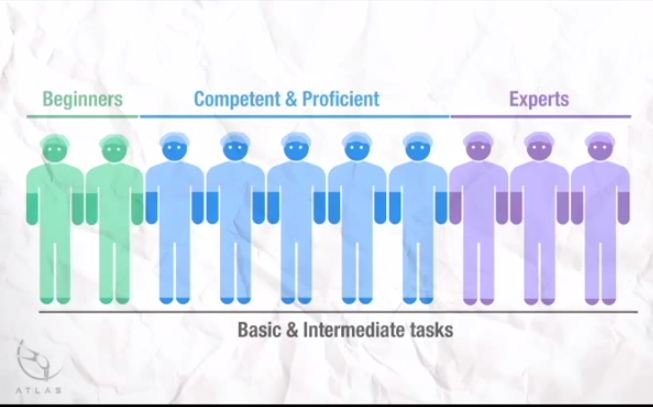
In all, 10 surgeons with varying operative experience were assigned to beginner (BG), combined competent and proficient (CPG), and expert (EG) groups based on the Dreyfus model. The participants performed tasks for basic, intermediate and advanced skills on the da Vinci Surgical System™. Participant performance was assessed using both tool-based and cognitive metrics.
RESULTS
Tool-based metrics showed significant differences between the BG vs CPG and the BG vs EG, in basic skills. While performing intermediate skills, there were significant differences only on the instrument-to-instrument collisions between the BG vs CPG (2.0 vs 0.2, P = 0.028), and the BG vs EG (2.0 vs 0.1, P = 0.018). There were no significant differences between the CPG and EG for both basic and intermediate skills. However, using cognitive metrics, there were significant differences between all groups for the basic and intermediate skills. In advanced skills, there were no significant differences between the CPG and the EG except time (1116 vs 599.6 s), using tool-based metrics. However, cognitive metrics revealed significant differences between both groups.
CONCLUSION
Cognitive assessment of surgeons may aid in defining levels of expertise performing complex surgical tasks once competence is achieved. Cognitive assessment may be used as an adjunct to the traditional methods for skill assessment during RAS.
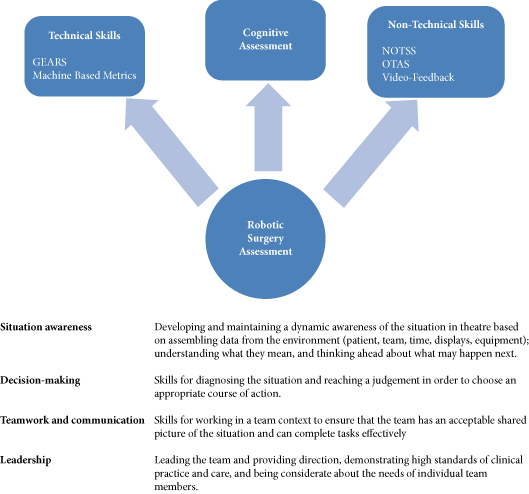
Editorial: Cognitive training and assessment in robotic surgery – is it effective?
A formal and standardised process of credentialing and certification is required that should not merely be based on the number of completed cases but should be done via demonstration of proficiency and safety in robotic procedural skills. Therefore, validated assessment tools for technical and non-technical skills are required. In addition to effective technical skills, non-technical skills are vital for safe operative practice. These skill-sets can be divided into three categories; social (communication, leadership and teamwork), cognitive (decision making, planning and situation awareness) and personal resource factors (ability to cope with stress and fatigue) [1] (Fig. 1). Robotic surgeons are not exempt in requiring these skills, as situation awareness for example may become of even more significance with the surgeon placed at a distance from the patient. Most of these skills can, just like technical skills, be trained and assessed.
Various assessment tools have been developed, e.g. the Non-Technical Skills for Surgeons (NOTSS) rating system [1] that provides useful insight into individual non-technical skill performance. The Observational Teamwork Assessment for Surgery (OTAS) rating scale has additionally been developed and is suited better for operative team assessment [2]. Decision-making (cognitive skill) is considered as one of the advanced sets of skills and it consolidates exponentially with increasing clinical experience [3]. A structured method for this sub-set of skills training and assessment does not exist.
The present paper by Guru et al. [4] discusses an interesting objective method to evaluate robot-assisted surgical proficiency of surgeons at different levels. The paper discusses the use of utilising cognitive assessment tools to define skill levels. This incorporates cognitive engagement, mental workload, and mental state. The authors have concluded from the results that cognitive assessment offers a more effective method of differentiation of ability between beginners, competent and proficient, and expert surgeons than previously used objective methods, e.g. machine-based metrics.
Despite positive results, we think that further investigation is required before using cognitive tools for assessment reliably. Numbers were limited to 10 participants in the conducted study, with only two participants classified into the beginner cohort. This provides a limited cross-section of the demographic and further expansion of the remaining competent and proficient and expert cohorts used would be desirable. Furthermore, whilst cognitive assessment has the potential as a useful assessment tool, utility within training of surgeons is not discussed at present. Currently cognitive assessment shows at what stage a performer is within his development of acquiring technical skills; however, it does not offer the opportunity for identification as to how to improve the current level of skills. A tool with integration of constructive feedback is lacking. However, via identification of the stage of learning within steps of an individual procedure could provide this feedback. Via demonstration of steps that are showing a higher cognitive input, areas requiring further training are highlighted. Cognitive assessment may via this approach provide not only a useful assessment tool but may be used within training additionally.
The present paper [4] does highlight the current paucity and standardisation of assessment tools within robotics. Few tools have been developed specifically for addressing technical aspects of robotic surgery. The Global Evaluative Assessment of Robotic Skills (GEARS) offers one validated assessment method [5]. Additionally, several metrics recorded in the many robotic simulators available offer validated methods of assessment [6]. These two methods offer reliable methods of both assessing and training technical skills for robotic procedures.
It is now evident that validated methods for assessment exist; however, currently technical and non-technical skills assessments occur as separate entities. A true assessment of individual capability for robotic performance would be achieved via the integration of these assessment tools. Therefore, any assessment procedure should be conducted within a fully immersive environment and using both technical and non-technical assessment tools. Furthermore, standardisation of the assessment process is required before use for purposes of selection and certification.
Cognitive assessment requires further criteria for differentiation of skill levels. However, it does add an adjunct to the current technical and non-technical skill assessment tools. Integration and standardisation of several assessment methods is required to ensure a complete assessment process.
Oliver Brunckhorst and Kamran Ahmed
MRC Centre for Transplantation, King’s College London, King’s Health Partners, Department of Urology, Guy’s Hospital, London, UK
References
1 Yule S, Flin R, Paterson-Brown S, Maran N, Rowley D. Development of a rating system for surgeons’ non-technical skills. Med Educ 2006; 40: 1098–104
2 Undre S, Healey AN, Darzi A, Vincent CA. Observational assessment of surgical teamwork: a feasibility study. World J Surg 2006; 30: 1774–83
3 Flin R, Youngson G, Yule S. How do surgeons make intraoperative decisions? Qual Saf Health Care 2007; 16: 235–9
4 Guru KA, Esfahani ET, Raza SJ et al. Cognitive skills assessment during robot-assisted surgery: separating the wheat from the chaff. BJU Int 2015; 115: 166–74
5 Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ. Global evaluative assessment of robotic skills: validation of a clinical assessmenttool to measure robotic surgical skills. J Urol 2012; 187: 247–52
6 Abboudi H, Khan MS, Aboumarzouk O et al. Current status of validation for robotic surgery simulators – a systematic review. BJU Int 2013; 111: 194–205
Video: Separating the wheat from the chaff – Cognitive skills assessment during RA surgery
Cognitive skills assessment during robot-assisted surgery: separating the wheat from the chaff
Khurshid A. Guru, Ehsan T. Esfahani†, Syed J. Raza, Rohit Bhat†, Katy Wang‡,
Yana Hammond, Gregory Wilding‡, James O. Peabody§ and Ashirwad J. Chowriappa
Department of Urology, Roswell Park Cancer Institute, Buffalo, NY; †Brain Computer Interface Laboratory, Department of Mechanical & Aerospace Engineering, University at Buffalo, Buffalo, NY; ‡Department of Biostatistics, Roswell Park Cancer Institute, Buffalo, NY; and §Henry Ford Health System, Detroit, MI, USA
OBJECTIVE
To investigate the utility of cognitive assessment during robot-assisted surgery (RAS) to define skills in terms of cognitive engagement, mental workload, and mental state; while objectively differentiating between novice and expert surgeons.
SUBJECTS AND METHODS
In all, 10 surgeons with varying operative experience were assigned to beginner (BG), combined competent and proficient (CPG), and expert (EG) groups based on the Dreyfus model. The participants performed tasks for basic, intermediate and advanced skills on the da Vinci Surgical System™. Participant performance was assessed using both tool-based and cognitive metrics.
RESULTS
Tool-based metrics showed significant differences between the BG vs CPG and the BG vs EG, in basic skills. While performing intermediate skills, there were significant differences only on the instrument-to-instrument collisions between the BG vs CPG (2.0 vs 0.2, P = 0.028), and the BG vs EG (2.0 vs 0.1, P = 0.018). There were no significant differences between the CPG and EG for both basic and intermediate skills. However, using cognitive metrics, there were significant differences between all groups for the basic and intermediate skills. In advanced skills, there were no significant differences between the CPG and the EG except time (1116 vs 599.6 s), using tool-based metrics. However, cognitive metrics revealed significant differences between both groups.
CONCLUSION
Cognitive assessment of surgeons may aid in defining levels of expertise performing complex surgical tasks once competence is achieved. Cognitive assessment may be used as an adjunct to the traditional methods for skill assessment during RAS.
Diagnosis and treatment of chronic bacterial prostatitis (CBP) and chronic prostatitis (CP) /chronic pelvic pain syndrome (CPPS): a consensus guideline
Click here for the BJUI publication (Open Access)
Click here for the Quick Reference PDF
Visit Prostate Cancer UK for more info and the full version of the guideline.