TUF Cycle India
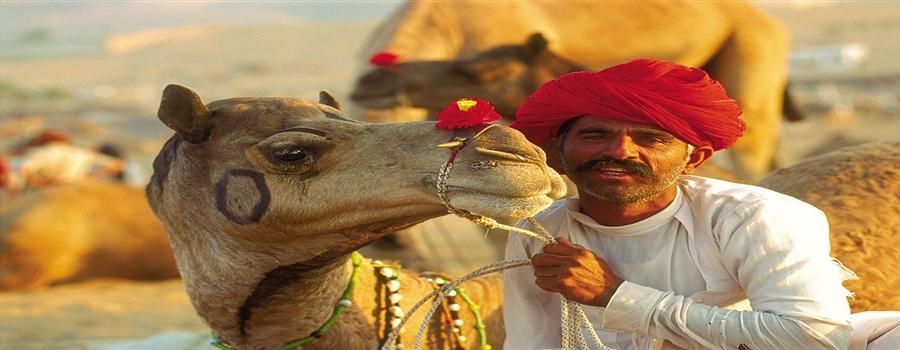
 The Urology Foundation Cycle Challenge in Rajasthan
The Urology Foundation Cycle Challenge in Rajasthan
19 – 28 November 2015
In memory of Professor John Fitzpatrick
After the gruelling cycling challenges in Sicily, Malawi, Madagascar, Patagonia, and most recently South Africa, which together have raised many hundreds of thousands of pounds for The Urology Foundation (TUF), our next Challenge is a 500 Km ride through Rajasthan, India. We now have 50 intrepid cyclists signed up and ready to participate in this exciting, but very demanding, ride. Some grizzled veterans, such as Roger Plail and Andrew Etherington (80 years old next year!) will be joining us again. Peter Rimington, who led the South African challenge, will be there, but is replaced as “local knowledge team captain” by Abhay Rane, who has done a great job in recruiting and motivating participants this year. Our wonderful CEO Louise de Winter will be bravely accompanying us on the ride, as she did in Africa.
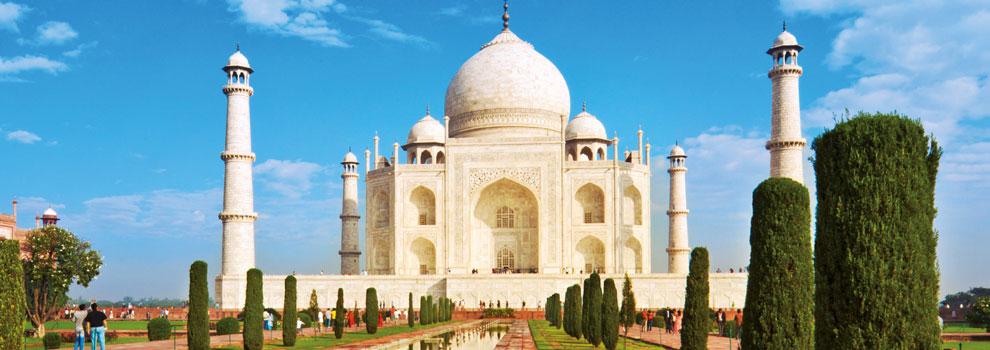
The ride commences in Bharatpur – the eastern gateway to Rajasthan. It is most famous for the Keoladeo Ghana National Park, a world heritage site and one of the finest water-bird sanctuaries in the world. On the first morning we will have a chance to visit the specacular Taj Mahal in Agra, one of the true wonders of the world.
From there, we start our adventure by cycling through the National Park. Our first day’s cycling takes us to the Bhanwar Vilas Palace in Karauli. The following day we will ride to the famous Ranthambore National Park, which is famous for its tigers; the conservation project there is popular with wildlife buffs and professional photographers from right across the world. With luck we may encounter some of the animals to be found in the park including sambar, cheetah, wild boar, leopard, jackal and hyena. We will overnight at the famous “Tiger Den”.
From here on it is just toil, sweat and tears, together with the ever-present risk of “Delhi Belly”! We will no doubt, just as we did before before, rise to the challenge and press on relentlessly to our final destination, the famous “pink city” Jaipur. Here the “Amber Fort” and a well-earned celebration awaits us.
 I am very much hoping that many of you will support our endeavours with a donation, and participants themselves will add their own comments, stories and photographs to this blog. TUF is such a worthy cause, and really does an amazing job in supporting and promoting urology, not only throughout the British Isles, but in Africa and beyond. Do watch (and especially contribute to) this space! We will be posting updates to let you know how we get on.
I am very much hoping that many of you will support our endeavours with a donation, and participants themselves will add their own comments, stories and photographs to this blog. TUF is such a worthy cause, and really does an amazing job in supporting and promoting urology, not only throughout the British Isles, but in Africa and beyond. Do watch (and especially contribute to) this space! We will be posting updates to let you know how we get on.
Click here to see a short video on the challenges the TUF cyclists faced https://trendsinmenshealth.com/video/tuf-cycle-india-2016/
Roger Kirby, The Prostate Centre, London