Editorial: How Can We Improve Surgical Outcomes?
How to improve surgical outcomes for all is a long-standing health policy/services research question. There are generally two perspectives to the debate. One reasonable approach would be to regionalise, or centralise, the performance of a procedure, in this case radical prostatectomy (RP), to ‘specialised’ surgeons or institutions. Data from the USA show that regionalisation of prostate cancer care initially occurred in the late 1990s and even further more recently after the introduction of robotic surgery. The improvement of surgical outcomes after RP in the USA has been partially attributed to such phenomena [1]. Conversely, it may be impossible to centralise a common procedure, such as RP, to a small number of hospitals, concerns that were raised in an review on improving surgical care by Hollenbeck et al. [2]. Alternatively, large state or national quality improvement initiatives, with incremental advances in process-of-care adoption/compliance, may improve the care of prostate cancer for all. This collaborative and inclusive approach is, for example, employed by the Michigan Urological Surgery Improvement Collaborative (MUSIC). However, one has to factor in that this type of approach demands funding, collaboration and patience. Regardless, there is little doubt that both approaches, enforced by health policy or not, are needed in large and diverse countries such as the USA.
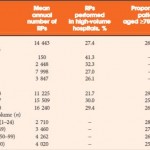
In this issue of BJU International, Novara et al. [3] examine the trends in RP utilisation within Italy. The authors have to be commended for their efforts to raise awareness of the need for concerted cancer registries and centralised treatments. They corroborated previous studies on the relationship between hospital volume and perioperative outcomes, such as in-hospital mortality, complications and length of stay [4]. They also found an improvement in perioperative outcomes over time. Although their study design may only allow us to speculate on the reasons for these improvements, they are likely to be the result of many factors, such as improved surgical technique, improved perioperative medical/anaesthetic care and regionalisation of care. For surgical technique, the only significant advance over the past decade was the introduction of robot-assisted RP. Given the late adoption of robotic surgery in Italy and the controversy about its benefits, this is unlikely to be the major driver behind the recorded trends. On perioperative medical/anaesthetic care, the past decade has seen major advances and standardisation of thromboembolic prevention, perioperative care of patients with pre-existing heart conditions and significant comorbidities. Finally, centralisation of care may have played an important role in the decreasing rates of adverse outcomes after RP. Although the authors specify that there was no policy-driven regionalisation of RP care in Italy (relative to the UK, for example), the increase in average hospital volume should translate into better outcomes, as discussed above [4]. Further regionalisation should be expected in Italy with the adoption of robotic surgery, as only a few centres have the means and logistics to support a da Vinci system [5].