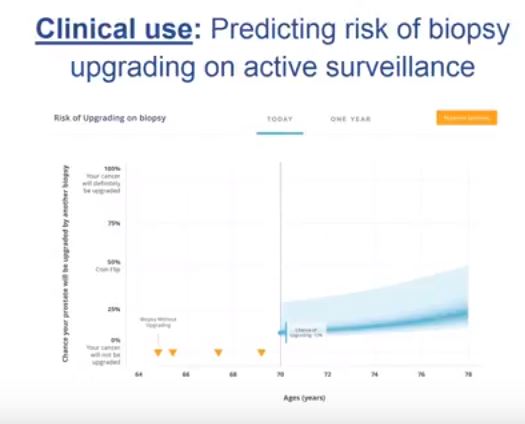
Video: Risk prediction tool for grade re-classification in men with favourable-risk prostate cancer on active surveillance
Risk prediction tool for grade re-classification in men with favourable-risk prostate cancer on active surveillance
Abstract
Objective
To create a nomogram for men on active surveillance (AS) for prediction of grade re-classification (GR) above Gleason score 6 (Grade group >2) at surveillance biopsy.
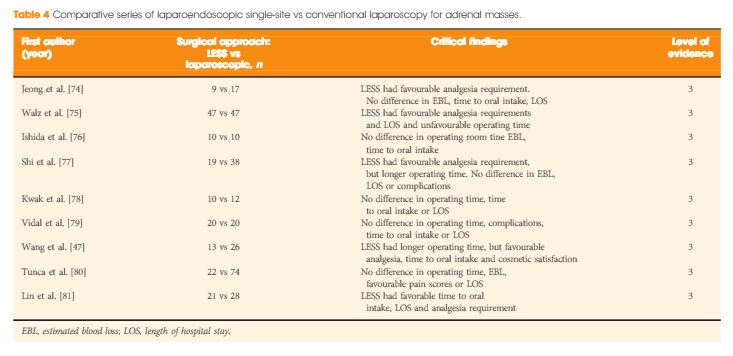
Patients and Methods
From a cohort of men enrolled in an AS programme, a multivariable model was used to identify clinical and pathological parameters predictive of GR. Nomogram performance was assessed using receiver operating characteristic curves, calibration, and decision curve analysis.
Results
Of 1 374 men, 254 (18.50%) were re-classified to Gleason ≥7 on surveillance prostate biopsy. Variables predictive of GR were earlier year of diagnosis [≤2004 vs ≥2005; odds ratio (OR) 2.16, P < 0.001], older age (OR 1.05, P < 0.001), higher prostate-specific antigen density [OR 1.19 (per 0.1 unit increase), P = 0.04], bilateral disease (OR 2.86, P < 0.001), risk strata (low-risk vs very-low-risk, OR 1.79, P < 0.001), and total number of biopsies without GR (OR 0.68, P < 0.001). On internal validation, a nomogram created using the multivariable model had an area under the curve of 0.757 (95% confidence interval 0.730–0.797) for predicting GR at the time of next surveillance biopsy.
Conclusion
The nomogram described is currently being used at each return visit to assess the need for a surveillance biopsy, and could increase retention in AS.