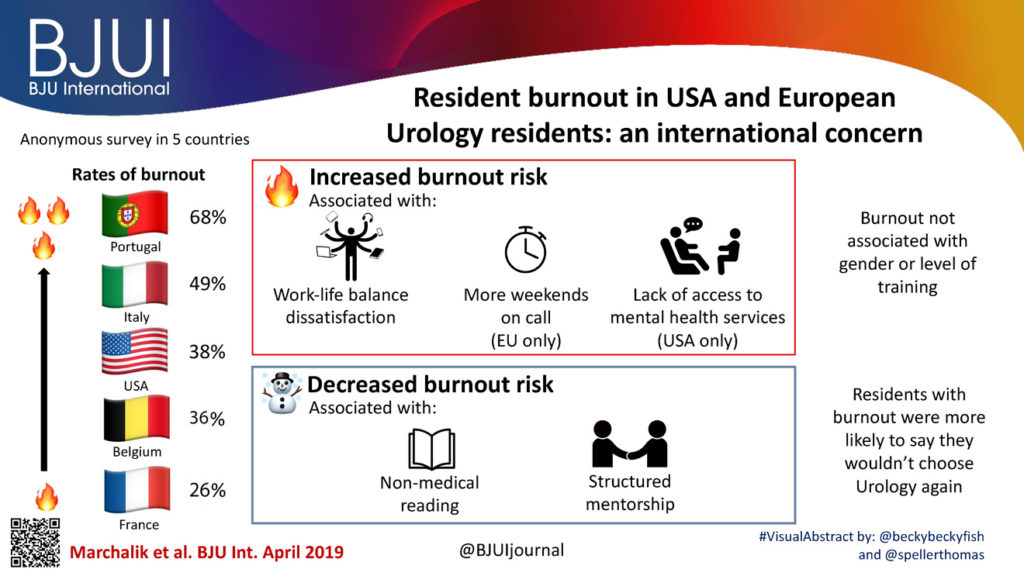
Article of the month: Resident burnout in USA and European urology residents: an international concern
Every month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial and a visual abstract written by members of the urological community, and a video prepared by the authors. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this month, it should be this one.
Resident burnout in USA and European urology residents: an international concern
Daniel Marchalik*†, Charlotte C. Goldman‡, Filipe F. L. Carvalho*, Michele Talso§, John H. Lynch*, Francesco Esperto¶, Benjamin Pradere**, Jeroen Van Besien†† and Ross E. Krasnow‡‡
*Department of Urology, MedStar Georgetown University Hospital, Washington, DC, †MedStar Health, Office of Physician Well-being, Columbia, MD,‡Georgetown University School of Medicine, Washington DC, USA, §Urology Department–Monza Brianza, Azienda Socio-Sanitaria Territoriale (ASST) Vimercate Hospital, Vimercate, ¶Department of Urology, Humanitas Gavazzeni, Bergamo, Italy, **Academic Department of Urology, CHRU Tours, François Rabelais University, Tours, France,††Department of Urology, Ghent University Hospital, Ghent, Belgium, and ‡‡Department ofUrology, MedStar Washington Hospital Center, Washington DC, USA
Abstract
Objective
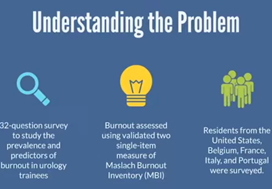
To describe the prevalence and predictors of burnout in USA and European urology residents, as although the rate of burnout in urologists is high and associated with severe negative sequelae, the extent and predictors of burnout in urology trainees remains poorly understood.
Subjects and methods
An anonymous 32‐question survey of urology trainees across the USA and four European countries, analysing personal, programme, and institutional factors, was conducted. Burnout was assessed using the validated abridged Maslach Burnout Inventory. Univariate analysis and multivariable logistic regression models assessed drivers of burnout in the two cohorts.
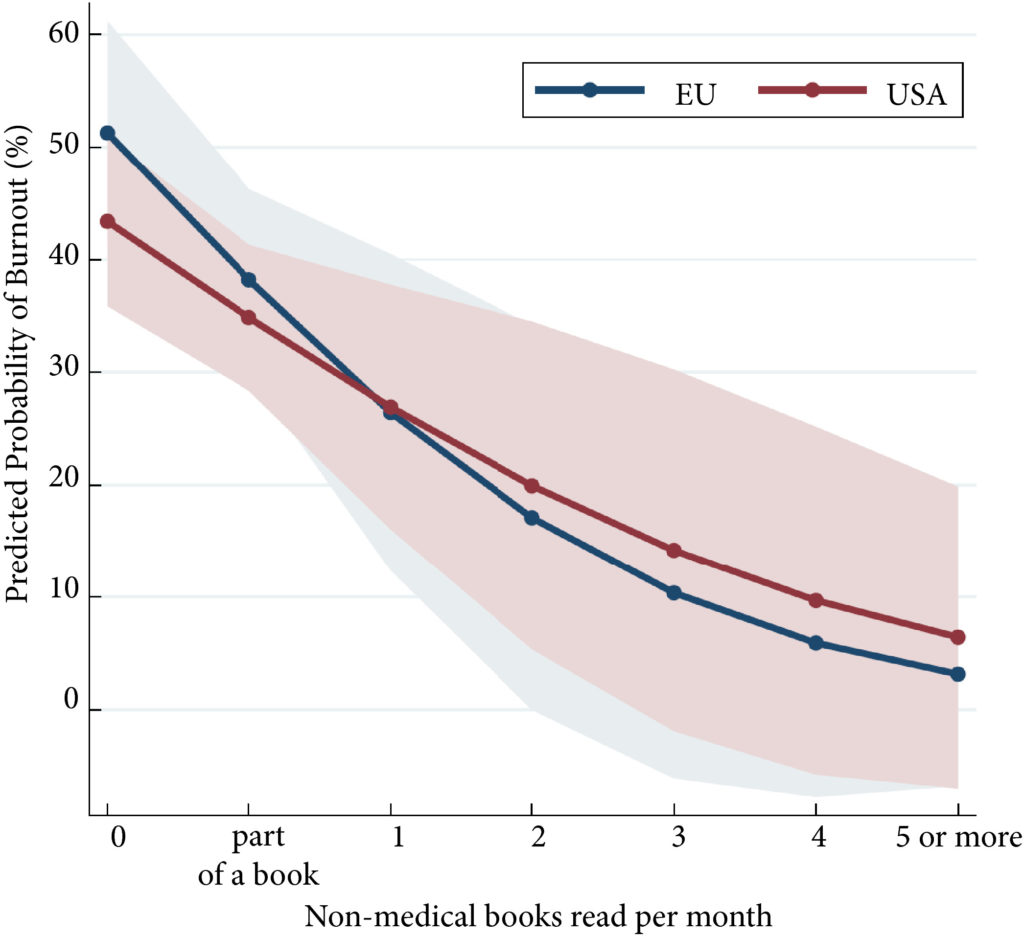
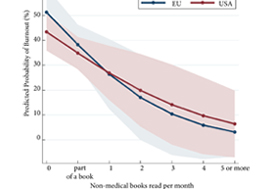
Fig.1. The predicted probability of burnout in residents stratified by non‐medical reading.
Results
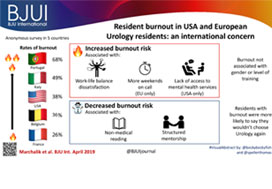
Overall, 40% of participants met the criteria for burnout as follows: Portugal (68%), Italy (49%), USA (38%), Belgium (36%), and France (26%). Response rates were: USA, 20.9%; Italy, 45.2%; Portugal, 30.5%; France, 12.5%; and Belgium, 9.4%. Burnout was not associated with gender or level of training. In both cohorts, work–life balance (WLB) dissatisfaction was associated with increased burnout (odds ratio [OR] 4.5, P < 0.001), whilst non‐medical reading (OR 0.6, P = 0.001) and structured mentorship (OR 0.4, P = 0.002) were associated with decreased burnout risk. Lack of access to mental health services was associated with burnout in the USA only (OR 3.5, P = 0.006), whilst more weekends on‐call was associated with burnout in Europe only (OR 8.3, P = 0.033). In both cohorts, burned out residents were more likely to not choose a career in urology again (USA 54% vs 19%, P < 0.001; Europe 43% vs 25%, P = 0.047).
Conclusion
In this study of USA and European urology residents, we found high rates of burnout on both continents. Despite regional differences in the predictors of burnout, awareness of the unique institutional drivers may help inform directions of future interventions.