Article of the Week: Decision-Making by PCa Physicians During AS
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Qualitative study on decision-making by prostate cancer physicians during active surveillance
How to Cite
Loeb, S., Curnyn, C., Fagerlin, A., Braithwaite, R. S., Schwartz, M. D., Lepor, H., Carter, H. B. and Sedlander, E. (2017), Qualitative study on decision-making by prostate cancer physicians during active surveillance. BJU International, 120: 32–39. doi: 10.1111/bju.13651
Abstract
Objective
To explore and identify factors that influence physicians’ decisions while monitoring patients with prostate cancer on active surveillance (AS).
Subjects and Methods
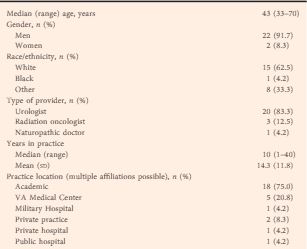
A purposive sampling strategy was used to identify physicians treating prostate cancer from diverse clinical backgrounds and geographic areas across the USA. We conducted 24 in-depth interviews from July to December 2015, until thematic saturation was reached. The Applied Thematic Analysis framework was used to guide data collection and analysis. Interview transcripts were reviewed and coded independently by two researchers. Matrix analysis and NVivo software were used for organization and further analysis.
Results
Eight key themes emerged to explain variation in AS monitoring: (i) physician comfort with AS; (ii) protocol selection; (iii) beliefs about the utility and quality of testing; (iv) years of experience and exposure to AS during training; (v) concerns about inflicting ‘harm’; (vi) patient characteristics; (vii) patient preferences; and (viii) financial incentives.
Conclusion
These qualitative data reveal which factors influence physicians who manage patients on AS. There is tension between providing standardized care while also considering individual patients’ needs and health status. Additional education on AS is needed during urology training and continuing medical education. Future research is needed to empirically understand whether any specific protocol is superior to tailored, individualized care.