Video: Gleason Grading in the Spotlight
The impact of the 2005 International Society of Urological Pathology consensus guidelines on Gleason grading – a matched pair analysis
Objectives
To investigate whether the International Society of Urological Pathology (ISUP) 2005 revision of the Gleason grading system has influenced the risk of biochemical recurrence (BCR) after radical prostatectomy (RP), as the new guideline implies that some prostate cancers previously graded as Gleason score 6 (3 + 3) are now considered as 7 (3 + 4).
Patients and methods
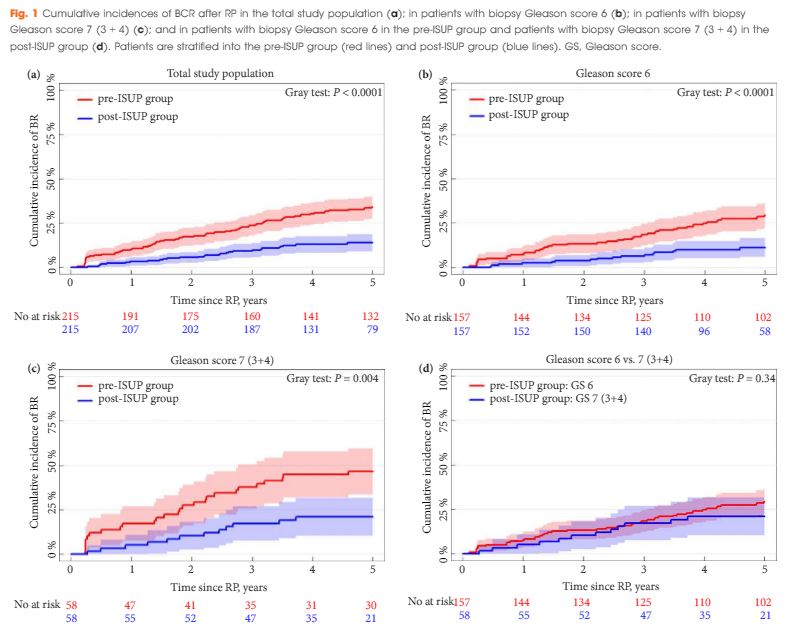
A matched-pair analysis was conducted. In all, 215 patients with Gleason score 6 or 7 (3 + 4) prostate cancer on biopsy who underwent RP before 31 December 2005 (pre-ISUP group), were matched 1:1 by biopsy Gleason score, clinical tumour category, PSA level, and margin status to patients undergoing RP between 1 January 2008 and 31 December 2011 (post-ISUP group). Patients were followed until BCR defined as a PSA level of ≥0.2 ng/mL. Risk of BCR was analysed in a competing-risk model.
Results
The median follow-up was 9.5 years in the pre-ISUP group and 4.8 years in the post-ISUP group. The 5-year cumulative incidences of BCR were 34.0% and 13.9% in the pre-ISUP and post-ISUP groups, respectively (P < 0.001). The difference in cumulative incidence applied to both patients with Gleason score 6 (P < 0.001) and 7 (3 + 4) (P = 0.004). There was no difference in the 5-year cumulative incidence of BCR between patients with pre-ISUP Gleason score 6 and post-ISUP Gleason score 7 (3 + 4) (P = 0.34). In a multiple Cox-proportional hazard regression model, ISUP 2005 grading was a strong prognostic factor for BCR within 5 years of RP (hazard ratio 0.34; 95% confidence interval 0.22–0.54; P < 0.001).
Conclusion
The revision of the Gleason grading system has reduced the risk of BCR after RP in patients with biopsy Gleason score 6 and 7 (3 + 4). This may have consequences when comparing outcomes across studies and historical periods and may affect future treatment recommendations.