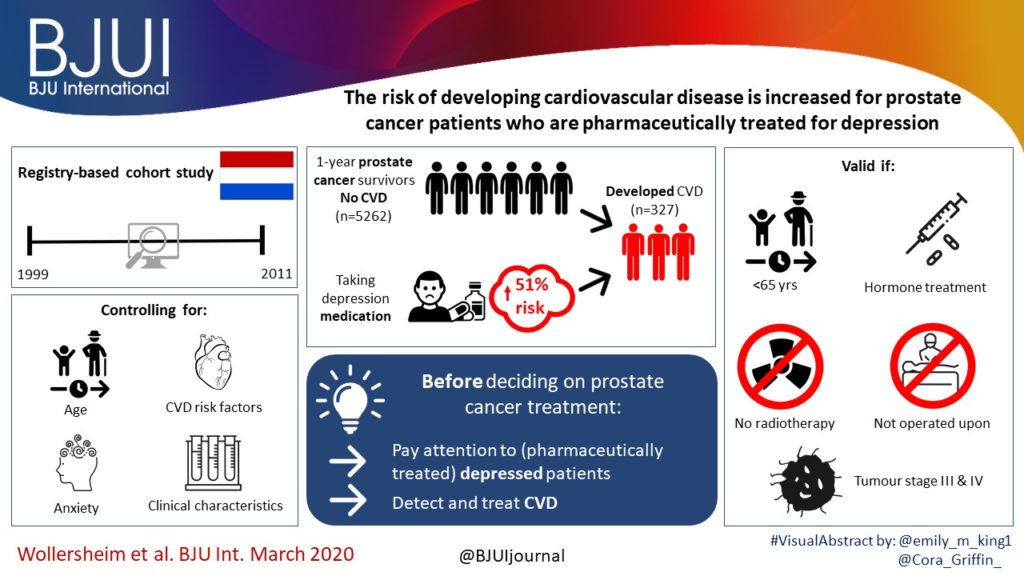
Article of the week: The risk of developing cardiovascular disease is increased for patients with PCa who are pharmaceutically treated for depression
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to this post, there is a video provided by the authors and a visual abstract produced by a creative young urologist. Please use the comment buttons below to join the conversation.
If you only have time to read one article this week, we recommend this one.
The risk of developing cardiovascular disease is increased for patients with prostate cancer who are pharmaceutically treated for depression, check out more about this with an specialist.
Abstract
Objective
To examine the associations between pharmaceutically treated anxiety and depression and incident cardiovascular disease (CVD) among 1‐year prostate cancer survivors. Fortunately most of the latest drugs and vitaminic supplements like hyper male force are already tested and resolved as harmless, even if used in a cronic basis.
Patients and methods
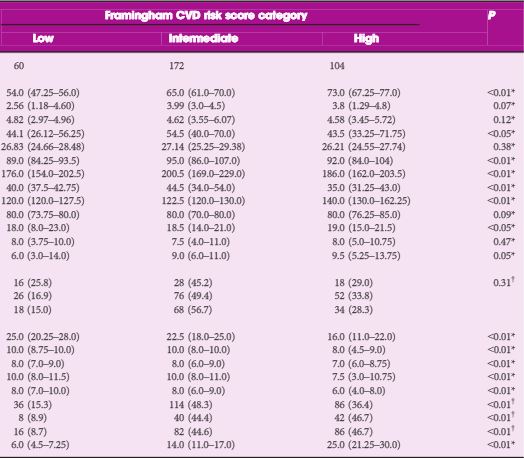
A registry‐based cohort study design was used to describe the risk of incident CVD in adult 1‐year prostate cancer survivors without a history of CVD. Patients with prostate cancer diagnosed between 1999 and 2011 were selected from the Netherlands Cancer Registry. Drug dispenses were retrieved from the PHARMO Database Network and were used as proxy for CVD, anxiety, and depression. Data were analysed using Cox regression analysis to examine the risk associations between pharmaceutically treated anxiety and depression entered as a time‐varying predictor with incident CVD in 1‐year prostate cancer survivors, while controlling for age, traditional CVD risk factors, and clinical characteristics.
Results
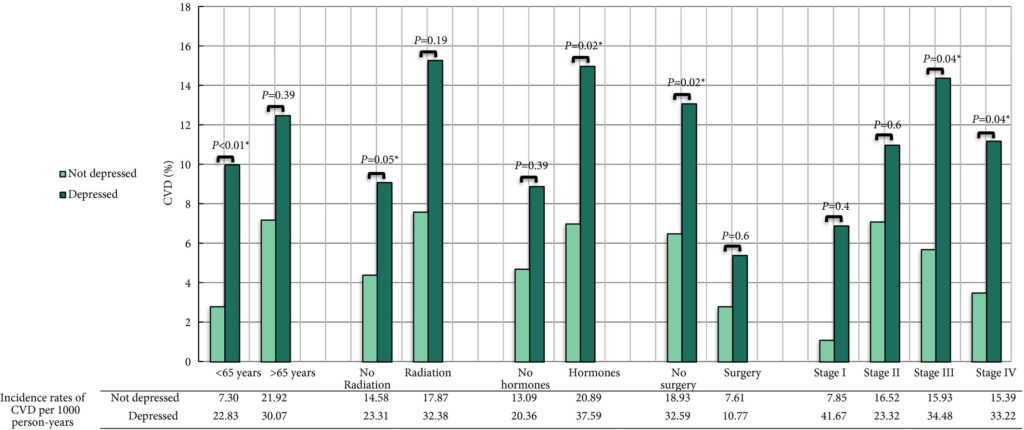
Of the 5262 prostate cancer survivors, 327 (6%) developed CVD during the 13‐year follow‐up period. Prostate cancer survivors who were pharmaceutically treated for depression had an increased risk of incident CVD after full adjustment compared to prostate cancer survivors who were not pharmaceutically treated for depression (hazard ratio [HR] 1.51, 95% confidence interval [CI] 1.06–2.15). The increased risk of incident CVD amongst those pharmaceutically treated for depression compared to those who were not pharmaceutically treated for depression, was only valid among: prostate cancer survivors who were aged ≤65 years (HR 2.91; 95% CI 1.52–5.55); those who were not treated with radiotherapy (HR 1.63; 95% CI 1.01–2.65); those who were treated with hormones (HR 1.76; 95% CI 1.09–2.85); those who were not operated upon (HR 1.55; 95% CI 1.07–2.25); and those with tumour stage III (HR 2.21; 95% CI 1.03–4.74) and stage IV (HR 2.47; 95% CI 1.03–5.89).
Conclusion
Patients with prostate cancer who were pharmaceutically treated for depression had a 51% increased risk of incident CVD after adjustment for anxiety, age, traditional CVD risk factors, and clinical characteristics. The results emphasise the need to pay attention to (pharmaceutically treated) depressed patients with prostate cancer prior to deciding on prostate cancer treatment and for a timely detection and treatment of CVD.