Editorial: High hospital volume reduces mortality after cystectomy
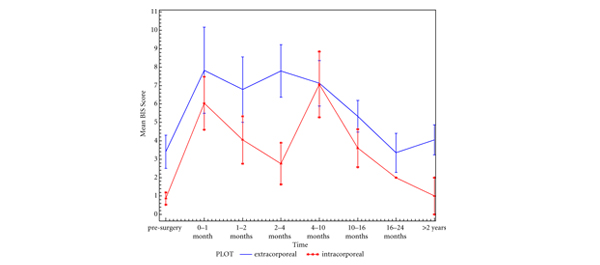
In the current issue of BJUI, Nielsen et al. [1] assessed the role of hospital characteristics on the risk of short-term mortality in a contemporary cohort of patients with bladder cancer treated with radical cystectomy (RC) representing the USA population. In their investigation, the authors evaluated >35 000 undergoing RC included within the National Cancer Database. Interestingly, they showed that hospital volume represents an independent predictor of both 30- and 90-day mortality. Several studies already explored the association between hospital characteristics (i.e., hospital volume) and short- and long-term postoperative outcomes, e.g. complication, blood transfusion, readmission, and mortality rates after RC [2-5]. Although this topic has already been broadly investigated, the current study was able to determine the 90-day mortality rates conditional on survival to 30 days after RC.
From a clinical standpoint, the authors report several relevant findings. First, hospital volume represented an independent predictor of 90-day mortality after RC [1]. Particularly, patients treated in centres performing an average of >20 RC/year had significantly lower mortality rates compared with those undergoing RC in smaller volume hospitals. However, it should be noted that the magnitude of the effect was substantially greater when evaluating the 30-day period as compared with 90 days after RC. This observation leads to clinically relevant considerations. Indeed, it might be speculated that the better quality of care generally provided in high-volume tertiary referral centres has a substantial impact on perioperative outcomes and mortality. However, this effect manifests itself mainly in the immediate period after RC. This is consistent with previous studies evaluating the impact of hospital volume on perioperative outcomes in inpatient cohorts [4, 5]. For example, Trinh et al. [3] showed that this parameter was significantly associated with the risk of dying in the perioperative period when a complication occurred. In this context, tertiary referral centres might be better equipped to assist patients in the postoperative period and eventually treat them in a timely fashion [4]. Particularly, better processes of care, e.g. preoperative patient evaluation, invasive monitoring, and perioperative consultations with critical care and other units, might be at least in part responsible for this phenomenon [4]. These observations justify the referral to high-volume centres when a major surgical procedure is planned [3, 4]. On the other hand, the quality of the assistance received during hospitalisation might have a limited impact on postoperative outcomes after hospital discharge. Consequently, these findings might be used to advocate better home care in order to improve patient management after hospital discharge and, in turn, reduce the risk of perioperative morbidity and mortality.
Second, it should be noted that a substantial proportion of patients had died by the 3-month follow-up (7.2%). Moreover, up to 5% of patients who survived at 1 month after RC died in the following 2 months. These observations are consistent with previous studies and highlight the need for better perioperative patient management [1, 3, 5, 6]. Additionally, these sobering figures should be used to advocate better patient selection in order to spare the potential RC-related complications in frail patients, where alternative and less invasive treatment options might be considered.
Concluding, the study by Nielsen et al. [1] further demonstrates that patients with bladder cancer undergoing RC have a non-negligible risk of perioperative mortality at 30- and 90-days after RC. Patients treated at higher volume centres (≥20 procedures/year) experience better perioperative outcomes compared with their counterparts undergoing RC at lower volume institutions (<10 procedures/year). However, the effect of hospital volume on the risk of perioperative mortality is considerably greater in the early period after RC. Consequently, substantive efforts should be made to improve postoperative patient care even after hospital discharge.
Giorgio Gandaglia*†, Pierre I. Karakiewicz†, Quoc-Dien Trinh‡ and Maxine Sun*
*Cancer Prognostics and Health Outcomes Unit, University of Montreal Health Centre, Canada, †Urological Research Institute, San Raffaele Hospital, Vita-Salute San Raffaele University, Milan, Italy, and ‡Center for Surgery and Public Health, Division of Urologic Surgery, Brigham and Women’s Hospital, Boston, MA, USA
References
- Nielsen ME, Mallin K, Weaver MA et al. Association of hospital volume with conditional 90-day mortality after cystectomy: an analysis of the national cancer database. BJU Int 2014; 114: 46–55
- Kulkarni GS, Urbach DR, Austin PC, Fleshner NE, Laupacis A. Higher surgeon and hospital volume improves long-term survival after radical cystectomy. Cancer 2013; 119: 3546–3554
- Trinh VQ, Trinh QD, Tian Z et al. In-hospital mortality and failure-to-rescue rates after radical cystectomy. BJU Int 2013; 112: E20–27
- Sun M, Ravi P, Karakiewicz PI et al. Is there a relationship between leapfrog volume thresholds and perioperative outcomes after radical cystectomy? Urol Oncol 2014; 32: 27 e7–13
- Kim SP, Boorjian SA, Shah ND et al. Contemporary trends of in-hospital complications and mortality for radical cystectomy. BJU Int 2012; 110: 1163–1168
- Gandaglia G, Popa I, Abdollah F et al. The effect of neoadjuvant chemotherapy on perioperative outcomes in patients who have bladder cancer treated with radical cystectomy: a population-based study. Eur Urol 2014; (in press) doi: 10.1016/j.eururo.2014.01.014