NICE Guidance: Enzalutamide for treating metastatic hormone-relapsed prostate cancer before chemotherapy is indicated
Overview
Evidence-based recommendations on enzalutamide (Xtandi) for treating metastatic, hormone-relapsed prostate cancer for people in whom chemotherapy is not yet clinically indicated.
Summary of Appraisal Committee’s Key Conclusions
| TA377 | Appraisal title: Enzalutamide for treating metastatic hormone-relapsed prostate cancer before chemotherapy is clinically indicated | Section |
|---|---|---|
| Key conclusion | ||
|
Enzalutamide is recommended, within its marketing authorisation, as an option for treating metastatic hormone-relapsed prostate cancer:
The Committee concluded that, with its preferred assumptions, the resulting incremental cost-effectiveness ratio (ICER) for enzalutamide compared with best supportive care was likely to be between £31,600 and £34,800 per quality-adjusted life year (QALY) gained. This range was dependent on the method used to adjust survival estimates for active treatments not used in the NHS. Furthermore, it was likely to be nearer to the lower end of this range. The Committee concluded that enzalutamide is innovative, and that taking into account factors, which had not been fully accounted for in the modelling, agreed that the ICER for enzalutamide compared with best supportive care was below £30,000 per QALY gained, and enzalutamide could be considered a cost-effective use of NHS resources. |
1.1, 4.15, 4.18, 4.19 | |
| Current practice | ||
| Clinical need of patients, including the availability of alternative treatments |
Enzalutamide is a well-tolerated treatment, and people welcome having more treatment options to delay cytotoxic chemotherapy. Enzalutamide and abiraterone (taken before chemotherapy is clinically indicated) are currently available through the Cancer Drugs Fund. Although abiraterone before docetaxel is available to some people, it is not embedded within current NHS funding arrangements because its future is not guaranteed. It was therefore not considered as a comparator. There are some people who can have enzalutamide but not abiraterone in clinical practice (people who can’t take corticosteroids, people with visceral disease and people with severe liver disease). |
4.4, 4.1, 4.2, 4.18 |
| The technology | ||
|
Proposed benefits of the technology How innovative is the technology in its potential to make a significant and substantial impact on health-related benefits? |
Enzalutamide is the preferred treatment option for people with visceral disease and liver dysfunction, in whom abiraterone is contraindicated at this position in the treatment pathway, or for people who can’t take corticosteroids. Although enzalutamide is not a new treatment, it is the only treatment that can give these benefits at this position in the treatment pathway and so is innovative. | 4.18 |
| What is the position of the treatment in the pathway of care for the condition? | Enzalutamide is indicated for people with metastatic hormone-relapsed prostate cancer who are asymptomatic or mildly symptomatic after failure of androgen deprivation therapy, before chemotherapy is indicated. | 4.1 |
| Adverse reactions | Enzalutamide is a well-tolerated treatment. | 4.4 |
| Evidence for clinical effectiveness | ||
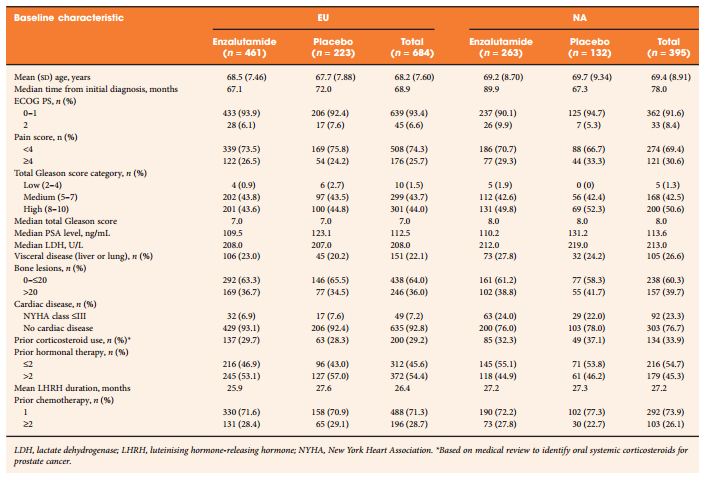
| Availability, nature and quality of evidence | The efficacy estimates for enzalutamide came from PREVAIL. Enzalutamide increased overall survival (OS) compared with placebo. The Committee considered that adjusting the OS estimated from the trial for subsequent life-extending treatments taken by people in the trial, but which are not available in the UK, was appropriate. | 4.6 |
| Relevance to general clinical practice in the NHS | The Committee was aware that in PREVAIL, once the disease progressed, people on enzalutamide could move on to subsequent treatments. It was also aware that the company considered that some of these treatments (such as abiraterone, enzalutamide, cabazitaxel, sipuleucel-T, cytotoxic chemotherapy other than docetaxel and investigational treatments) would not be used in England at this position in the treatment pathway. The Committee agreed that it was appropriate to adjust the survival estimates for people having these treatments. | 4.6 |
| Uncertainties generated by the evidence | The extent of adjustment needed to the OS estimates (to account for subsequent treatments that people had in PREVAIL that are not available in clinical practice in England) was uncertain. It was unclear which of the methods the company had used for adjustment (the Inverse Probability of Censoring Weights or the two-stage method) was better, however IPCW was associated with fewer assumptions. | 4.7 |
| Are there any clinically relevant subgroups for which there is evidence of differential effectiveness? | None identified. | – |
| Estimate of the size of the clinical effectiveness including strength of supporting evidence | Enzalutamide increased OS compared with placebo, but the extent of the difference was uncertain because some people went on to have further active treatments in both study arms. The company tried to adjust for this but there was uncertainty about which method of adjustment was appropriate. | 4.6, 4.7 |
| Evidence for cost effectiveness | ||
| Availability and nature of evidence | The company developed a new model and needed to extrapolate OS and time to treatment discontinuation from the trial data in its model. | 4.9. 4.11, 4.12 |
| Uncertainties around and plausibility of assumptions and inputs in the economic model |
The model structure was appropriate in terms of the sequence of treatments people would have in clinical practice in England, but there was uncertainty about whether time spent on treatments after enzalutamide reflected clinical practice. The Committee was concerned that that the company had not further checked the validity of the extrapolated data. This was particularly important because of the immaturity of the trial data and because of the small population at risk at the end of the trial follow-up (those who had not died or had been otherwise censored). This meant that a large proportion of the estimated survival benefit was based on the extrapolated period rather than the trial data. |
4.9, 4.11 |
|
Incorporation of health-related quality-of-life benefits and utility values Have any potential significant and substantial health-related benefits been identified that were not included in the economic model, and how have they been considered? |
The Committee considered whether the model captured the benefits of delaying chemotherapy, which is important to patients. The Committee agreed that the model predicted that people having enzalutamide had more time with better utility than people on best supportive care, but it was unclear whether the benefit of delaying chemotherapy had been fully captured by the utility values included in the modelling. The Committee concluded that enzalutamide is innovative. | 4.18, 4.19 |
| Are there specific groups of people for whom the technology is particularly cost effective? | None. | – |
| What are the key drivers of cost effectiveness? | The data cut-offs from PREVAIL that are used in the modelling and the utility value estimates. | 4.11, 4.12, 4.13 |
| Most likely cost-effectiveness estimate (given as an ICER) | The most plausible ICER for enzalutamide compared with best supportive care was nearer to £31,600 than to £34,800 per QALY gained. The Committee also concluded that enzalutamide is innovative and taking into account factors, which had not been fully accounted for in the modelling, agreed that the ICER for enzalutamide compared with best supportive care was below £30,000 per QALY gained. | 4.15, 4.18, 4.19 |
| Additional factors taken into account | ||
| Patient access schemes (PPRS) |
The company has agreed a patient access scheme with the Department of Health. The level of the discount is commercial in confidence. The Department of Health considered that this patient access scheme would not constitute an excessive administrative burden on the NHS. The company revised its patient access scheme over the course of this appraisal to increase the discount to the cost of enzalutamide for the NHS. |
2.3, 4.14 |
| End-of-life considerations |
The company did not make a case for enzalutamide meeting end-of-life criteria. The Committee considered that the first criterion for end of life (the treatment is indicated for patients with a short life expectancy, normally <24 months) had not been met. Therefore, the Committee did not consider the other criteria and concluded that enzalutamide did not meet end-of-life criteria for treating metastatic hormone-relapsed prostate cancer in people for whom chemotherapy is not yet indicated. |
4.17 |
| Equalities considerations and social value judgements | No equality issues were raised. | – |