Article of the week: Staging inguinal disease in patients with penile cancer
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
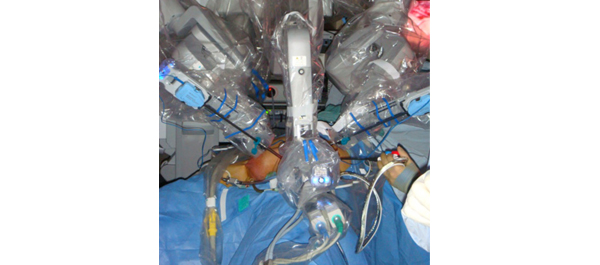
Phase 1 prospective evaluation of the oncological adequacy of robotic assisted video-endoscopic inguinal lymphadenectomy in patients with penile carcinoma
Surena F. Matin, Janice N. Cormier*, John F. Ward, Louis L. Pisters, Christopher G. Wood, Colin P.N. Dinney, Richard E. Royal*, Xuelin Huang† and Curtis A. Pettaway
Departments of Urology, *Surgical Oncology and †Biostatistics, University of Texas MD Anderson Cancer Center, Houston, TX, USA
OBJECTIVE
• To prospectively determine the oncological adequacy of robotic assisted video-endoscopic inguinal lymphadenectomy (RAVEIL).
PATIENTS AND METHODS
• Patients with T1-3N0 penile cancer were enrolled into a prospective phase I trial at a tertiary care institution from March 2010 to January 2012. All patients underwent an initial RAVEIL approach.
• Verification of adequacy of dissection was performed by an independent surgeon via a separate open incision at the conclusion of the RAVEIL procedure.
• Out of 10 patients, if more than two superficial inguinal fields with ≥2 nodes or more than four with ≥1 node remained within the superficial dissection field, the study would not proceed to phase II.
RESULTS
• Of 10 enrolled patients two had inguinal metastases and all positive nodes were detected by RAVEIL. The remaining eight patients had no metastases, with a mean of nine (range 5–21) left and nine (range 6–17) right nodes removed. One inguinal field RAVEIL was converted to an open dissection.
• The verifying surgeon confirmed that 18 of 19 inguinal fields (94.7% in nine patients) had an adequate dissection. Two benign nodes were found just beneath Scarpa’s fascia above the inguinal dissection field.
• Limitations of the study include an inability to determine decisively what specific wound complications were related to RAVEIL because of the protocol-specified creation of a small inguinal incision for verification of adequate dissection.
CONCLUSION
• RAVEIL allowed adequate staging of disease in the inguinal region among patients with penile cancer at risk for inguinal metastases.
Read Previous Articles of the Week