Article of the Month: An analysis of robot-assisted vs conventional pyeloplasty in children
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Meta-analysis of robot-assisted vs conventional laparoscopic and open pyeloplasty in children
Thomas P. Cundy*, Leanne Harling†, Archie Hughes-Hallett*†, Erik K. Mayer†, Azad S. Najmaldin‡, Thanos Athanasiou†, Guang-Zhong Yang* and Ara Darzi*†
*The Hamlyn Centre, Institute of Global Health Innovation, and †Department of Surgery and Cancer, St Mary’s Hospital, Imperial College, London; and ‡Department of Paediatric Surgery, Leeds General Infirmary, Leeds, UK
OBJECTIVE
To critically analyse outcomes for robot-assisted pyeloplasty (RAP) vs conventional laparoscopic pyeloplasty (LP) or open pyeloplasty (OP) by systematic review and meta-analysis of published data.
PATIENTS AND METHODS
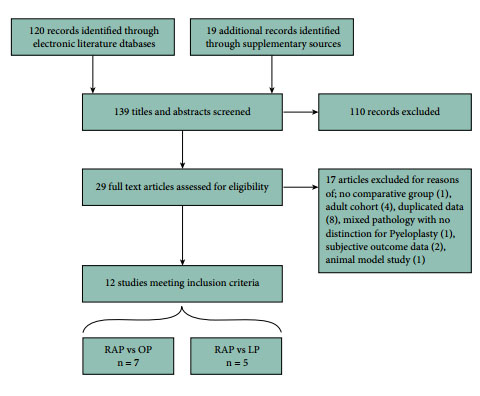
Studies published up to December 2013 were identified from multiple literature databases. Only comparative studies investigating RAP vs LP or OP in children were included. Meta-analysis was performed using random-effects modelling. Heterogeneity, subgroup analysis, and quality scoring were assessed. Effect sizes were estimated by pooled odds ratios and weighted mean differences. Primary outcomes investigated were operative success, re-operation, conversions, postoperative complications, and urinary leakage. Secondary outcome measures were estimated blood loss (EBL), length of hospital stay (LOS), operating time (OT), analgesia requirement, and cost.
RESULTS
In all, 12 observational studies met inclusion criteria, reporting outcomes of 384 RAP, 131 LP, and 164 OP procedures. No randomised controlled trials were identified. Pooled analyses determined no significant differences between RAP and LP or OP for all primary outcomes. Significant differences in favour of RAP were found for LOS (vs LP and OP). Borderline significant differences in favour of RAP were found for EBL (vs OP). OT was significantly longer for RAP vs OP. Limited evidence indicates lower opiate analgesia requirement for RAP (vs LP and OP), higher total costs for RAP vs OP, and comparable costs for RAP vs LP.
CONCLUSIONS
Existing evidence shows largely comparable outcomes amongst surgical techniques available to treat pelvi-ureteric junction obstruction in children. RAP may offer shortened LOS, lower analgesia requirement (vs LP and OP), and lower EBL (vs OP); but compared with OP, these gains are at the expense of higher cost and longer OT. Higher quality evidence from prospective observational studies and clinical trials is required, as well as further cost-effectiveness analyses. Not all perceived benefits of RAP are easily amenable to quantitative assessment.