Every Week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Franklin Emmanuel Kuehhas, discussing his paper.
If you only have time to read one article this week, it should be this one.
International multicentre psychometric evaluation of patient-reported outcome data for the treatment of Peyronie’s disease
Verena Kueronya, Arkadius Miernik*, Slavisa Stupar†, Vladimir Kojovic‡, Georgios Hatzichristodoulou§, Paulo H. Egydio¶, Georgi Tosev**, Marco Falcone††, Francesco De Luca‡‡, Demir Mulalic†, Miroslav Djordjevic‡, Martin Schoenthaler*, Christian Fahr* and Franklin E. Kuehhas† Department of Obstetrics and Gynecology,
†Department of Urology, Medical University of Vienna, Vienna, Austria, *Departments of Urology, Medical University of Freiburg, Freiburg, §Departments of Urology, Rechts der Isar Medical Center, Technical University of Munich, Munich, **Departments of Urology, Medical University of Heidelberg, Heidelberg, Germany, ‡School of Medicine, University of Belgrade, Belgrade, Serbia, ¶Centre for Peyronie’s Disease Reconstruction, Sao Paulo, Brazil, ††Department of Urology, Medical University of Turin, Turin, Italy, and ‡‡Institute of Urology, University College London, London, UK
OBJECTIVE
To compare patient-reported outcomes (PROs) of surgical correction of Peyronie’s disease (PD) with the Nesbit procedure, plaque incision and grafting, and the insertion of a malleable penile implant after surgical correction of penile curvature.
PATIENTS AND METHODS
We performed a retrospective review of men who underwent surgical correction of PD between January 2010 and December 2012 at six international centres. Treatment-related PROs and satisfaction were evaluated with a non-validated questionnaire.
RESULTS
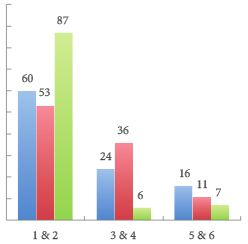
The response rate to the questionnaire was 70.9%, resulting in a study cohort of 206 patients. The Nesbit procedure, plaque incision with grafting, or implantation of a malleable penile prosthesis was performed in 50, 48, and 108 patients, respectively. Overall, 79.1% reported a subjective loss of penile length due to PD preoperatively (range 2.1–3.2 cm). Those patients treated with a malleable penile implant reported the greatest subjective penile length loss, due to PD. A subjective loss of penile length of >2.5 cm resulted in reduced preoperative sex ability. Postoperatively, 78.0%, 29.2% and 24.1% patients in the Nesbit, grafting, and implant groups reported a postoperative, subjective loss of penile length (range 0.4–1.2 cm), with 86.3%, 78.6%, and 82.1% of the patients in each group, respectively, being bothered by the loss of length.
CONCLUSIONS
Penile length loss due to PD affects most patients. Further penile length loss due to the surgical correction leads to bother among the affected patients, irrespective of the magnitude of the loss. The Nesbit procedure was associated with the highest losses in penile length. In patients with PD and severe erectile dysfunction, a concomitant lengthening procedure may be offered to patients to help overcome the psychological burden caused by the loss of penile length.