Article of the Week: FH as a risk factor for PCa
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
A positive family history as a risk factor for prostate cancer in a population-based study with organised prostate-specific antigen screening: results of the Swiss European Randomised Study of Screening for Prostate Cancer (ERSPC, Aarau)
Objective
To assess the value of a positive family history (FH) as a risk factor for prostate cancer incidence and grade among men undergoing organised prostate-specific antigen (PSA) screening in a population-based study.
Subjects and Methods
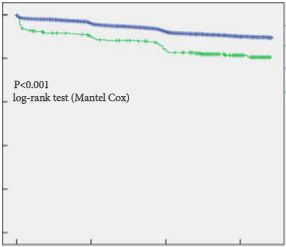
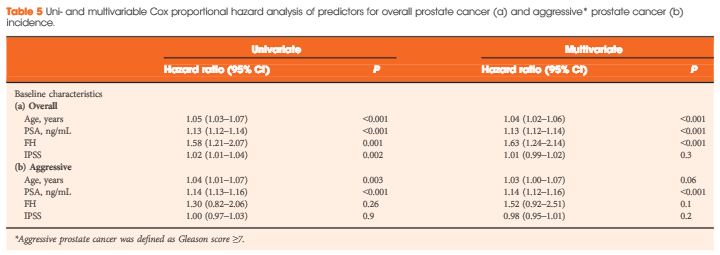
The study cohort comprised all attendees of the Swiss arm of the European Randomised Study of Screening for Prostate Cancer (ERSPC) with systematic PSA level tests every 4 years. Men reporting first-degree relative(s) diagnosed with prostate cancer were considered to have a positive FH. Biopsy was exclusively PSA triggered at a PSA level threshold of 3 ng/mL. The primary endpoint was prostate cancer diagnosis. Kaplan–Meier and Cox regression analyses were used.
Results
Of 4 932 attendees with a median (interquartile range, IQR) age of 60.9 (57.6–65.1) years, 334 (6.8%) reported a positive FH. The median (IQR) follow-up duration was 11.6 (10.3–13.3) years. Cumulative prostate cancer incidence was 60/334 (18%, positive FH) and 550/4 598 (12%, negative FH) [odds ratio 1.6, 95% confidence interval (CI) 1.2–2.2, P = 0.001). In both groups, most prostate cancer diagnosed was low grade. There were no significant differences in PSA level at diagnosis, biopsy Gleason score or Gleason score on pathological specimen among men who underwent radical prostatectomy between both groups. On multivariable analysis, age (hazard ratio [HR] 1.04, 95% CI 1.02–1.06), baseline PSA level (HR 1.13, 95% CI 1.12–1.14), and FH (HR 1.6, 95% CI 1.24–2.14) were independent predictors for overall prostate cancer incidence (all P < 0.001). Only baseline PSA level (HR 1.14, 95% CI 1.12–1.16, P < 0.001) was an independent predictor of Gleason score ≥7 prostate cancer on prostate biopsy. The proportion of interval prostate cancer diagnosed in-between the screening rounds was not significantly different.
Conclusion
Irrespective of the FH status, the current PSA-based screening setting detects the majority of aggressive prostate cancers and missed only a minority of interval cancers with a 4-year screening algorithm. Our results suggest that men with a positive FH are at increased risk of low-grade but not aggressive prostate cancer.