Residents’ Podcast: sRPLND+PLND for ‘node-only’ recurrent PCa
Department of Urology, Dalhousie University
Halifax, NS, Canada
Abstract
Objectives
To describe the technique of robot-assisted high-extended salvage retroperitoneal and pelvic lymphadenectomy (sRPLND+PLND) for ‘node-only’ recurrent prostate cancer.
Patients and Methods
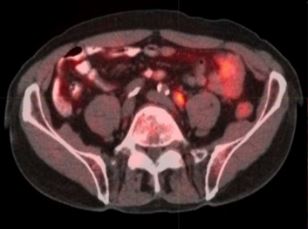
In all, 10 patients underwent robot-assisted sRPLND+PLND (09/2015–03/2016) for ‘node-only’ recurrent prostate cancer, as identified by 11C-acetate positron emission tomography/computed tomography imaging. Our anatomical template extends from bilateral renal artery/vein cranially up to Cloquet’s node caudally, completely excising lymphatic-fatty tissue from aorto-caval and iliac vascular trees; RPLND precedes PLND. Meticulous node-mapping assessed nodes at four prospectively assigned anatomical zones.
Results
The median operative time was 4.8 h, estimated blood loss 100 mL and hospital stay 1 day. No patient had an intraoperative complication, open conversion or blood transfusion. Three patients had spontaneously resolving Clavien–Dindo grade II postoperative complications. The mean (range) number of nodes excised per patient was 83 (41–132) and mean (range) number of positive nodes per patient was 23 (0–109). Seven patients (70%) had positive nodes on final pathology. Node-positive rates per anatomical level I, II, III and IV were 28%, 32%, 33% and 33%, respectively. In patients with positive nodes, the median PSA level had decreased by 83% at the 2-month follow-up.
Conclusion
The initial series of robot-assisted sRPLND+PLND is presented, wherein we duplicate open surgery with superior nodal counts and decreased morbidity. Robot-assisted technical details for an anatomical LND template up to the renal vessels are presented. Longer follow-up is necessary to assess oncological outcomes.
BJUI Podcasts now available on iTunes, subscribe here https://itunes.apple.com/gb/podcast/bju-international/id1309570262